Atrial Fibrillation Treatment: Common Medications, Alternatives, and What Works
When you have atrial fibrillation, an irregular and often rapid heart rhythm that can increase stroke risk. Also known as AFib, it doesn’t always cause symptoms—but it still needs careful management to prevent blood clots and heart damage. This isn’t just about taking a pill. It’s about choosing the right mix of drugs, lifestyle shifts, and sometimes procedures to keep your heart beating safely.
Most atrial fibrillation treatment, a strategy to restore normal heart rhythm or control heart rate while reducing stroke risk. Also known as AFib management, it breaks down into two main paths: rate control, slowing the heart rate to a safe level even if the rhythm stays irregular. Also known as heart rate management, it and rhythm control, trying to get the heart back into a normal beat pattern. Also known as cardioversion, it. Rate control is often the first move, especially for older patients or those with few symptoms. Rhythm control might be better if you’re younger, feel terrible when AFib hits, or have heart failure. The choice isn’t one-size-fits-all—it’s personal.
Then there’s the big one: blood thinners, medications that prevent clots from forming in the heart’s upper chambers. Also known as anticoagulants, they. If you have AFib, your stroke risk goes up—sometimes dramatically. That’s why doctors often recommend these drugs, even if your heart rhythm feels fine. Warfarin has been the go-to for decades, but newer options like apixaban, rivaroxaban, and dabigatran are now common. They don’t need constant blood tests, have fewer food interactions, and work just as well for most people. But they’re not for everyone. Kidney problems, bleeding history, or cost can change the game.
What you won’t find in every guide? The real trade-offs. Beta-blockers like metoprolol help with rate control but can leave you tired. Calcium channel blockers like diltiazem work fast but may drop your blood pressure too far. Antiarrhythmics like amiodarone can restore rhythm—but they come with lung, liver, and thyroid risks. And while some people look to natural fixes or supplements, there’s no proven alternative to approved meds when it comes to stroke prevention. Skipping your blood thinner because you read a blog post isn’t a risk worth taking.
You’ll also notice how often AFib ties into other conditions. High blood pressure? Thyroid issues? Sleep apnea? All of these can make AFib worse—or even trigger it. Treating them isn’t optional. It’s part of the treatment plan. That’s why some of the best guides here don’t just list drugs. They show how AFib connects to statins, diuretics, and even kidney function. Because managing AFib isn’t just about the heart—it’s about your whole body.
What you’ll find below isn’t a textbook. It’s real comparisons: how one blood thinner stacks up against another, why some meds work better for older adults, what happens when you mix AFib drugs with grapefruit or other common meds, and how lifestyle changes actually impact outcomes. No theory. No fluff. Just what people are using, what’s working, and what to watch out for.
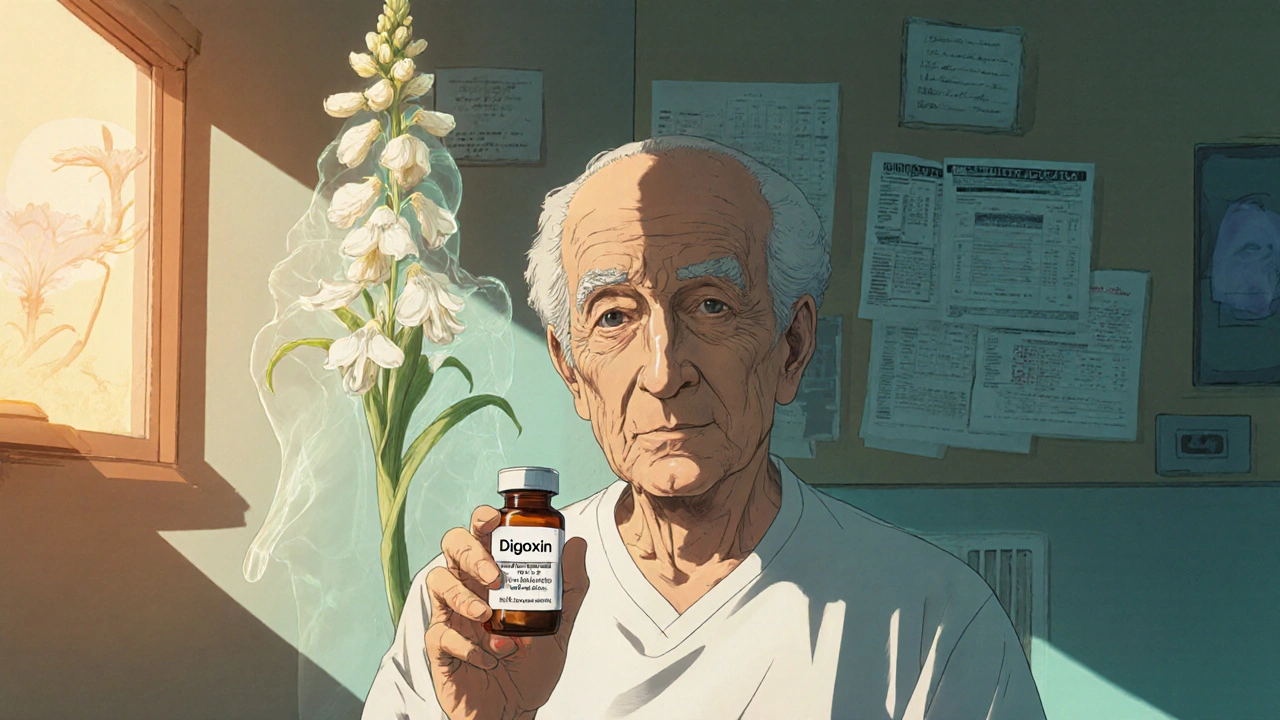
Digoxin vs Alternatives: What Works Best for Heart Failure and Atrial Fibrillation
Digoxin is still used for heart failure and atrial fibrillation, but newer drugs like SGLT2 inhibitors and ARNI offer better survival and fewer side effects. Learn how digoxin compares to alternatives and when to consider switching.