GAHT Drug Interaction Checker
How This Tool Works
Based on the latest research, this tool identifies potential interactions between your gender-affirming hormone therapy (GAHT) and medications you're taking. Remember: This is for informational purposes only and does not replace professional medical advice. Always consult your healthcare provider before making any medication changes.
Important Note: The article states that PrEP (tenofovir/emtricitabine) does not significantly interact with GAHT (<5% change in hormone levels). Newer HIV drugs like dolutegravir have minimal interactions. Always discuss changes with your provider.
When someone starts gender-affirming hormone therapy (GAHT), they’re not just changing their body-they’re starting a long-term medical journey. And like any long-term medication plan, it doesn’t happen in a vacuum. GAHT interacts with other drugs you might be taking. Some of these interactions are harmless. Others can be serious. Knowing what to watch for can mean the difference between feeling stable and safe-or facing unexpected side effects that throw your treatment off track.
How GAHT Works and Why Interactions Matter
Gender-affirming hormone therapy comes in two main forms: feminizing therapy for transgender women and nonbinary people assigned male at birth, and masculinizing therapy for transgender men and nonbinary people assigned female at birth. Feminizing therapy usually includes estradiol (a form of estrogen) and an anti-androgen like spironolactone or cyproterone acetate. Masculinizing therapy uses testosterone, delivered as gel, patches, or injections.
These hormones don’t just float around freely. Your body breaks them down using specific enzymes-mostly in the liver. The most important one is called CYP3A4. If another drug you’re taking affects this enzyme, it can change how fast or slow your body processes your hormones. That means your estradiol or testosterone levels could drop too low-or spike dangerously high.
And it’s not just about hormone levels. Some medications can make your body react differently to hormones. For example, if you’re on an antidepressant and start testosterone, your mood might change in ways you didn’t expect-even if your hormone levels look normal on paper. That’s because hormones and psychiatric drugs often share the same brain pathways.
Biggest Risks: HIV Medications and GAHT
Transgender people are at higher risk for HIV, so many are on antiretroviral therapy (ART). That’s where things get tricky.
Some HIV drugs, like efavirenz and nevirapine, are enzyme inducers. They speed up CYP3A4, which means your body clears estradiol faster. Studies show this can drop estrogen levels by 30-50%. That’s not just inconvenient-it can undo the physical changes you’ve worked hard for. You might notice breast tissue shrinking, mood swings returning, or hot flashes coming back.
On the flip side, drugs like cobicistat (used in combo pills like Stribild or Genvoya) block CYP3A4. This slows down estrogen breakdown. Estradiol levels can jump by 40-60% in just two weeks. That raises your risk of blood clots, stroke, or liver stress. One 2024 review of 1,843 transgender patients found that people on cobicistat-boosted regimens needed lower estradiol doses to avoid side effects.
The good news? Newer HIV drugs like dolutegravir (an integrase inhibitor) don’t interfere much. They might raise estradiol by 25-35%, but that’s usually not enough to require dose changes. If you’re starting or switching HIV meds, talk to your provider about checking your estradiol levels before and after the switch.
PrEP and GAHT: No Need to Worry
If you’re on PrEP (pre-exposure prophylaxis) to prevent HIV, you’ll be glad to know: it doesn’t interfere with GAHT. A major 2022 study followed 172 transgender people taking tenofovir/emtricitabine (Truvada or Descovy) while also on estrogen or testosterone. Hormone levels changed by less than 5%. Tenofovir levels stayed steady too.
This is huge. It means you don’t have to choose between protecting yourself from HIV and getting the hormones you need. You can do both safely. The study even used dried blood spot tests to confirm people were taking their meds correctly-92% stayed in the protective range.
One exception: long-acting cabotegravir injections (Apretude). There’s almost no data yet. Until more studies come out, stick with daily pills if you’re on GAHT. That’s the safest bet right now.
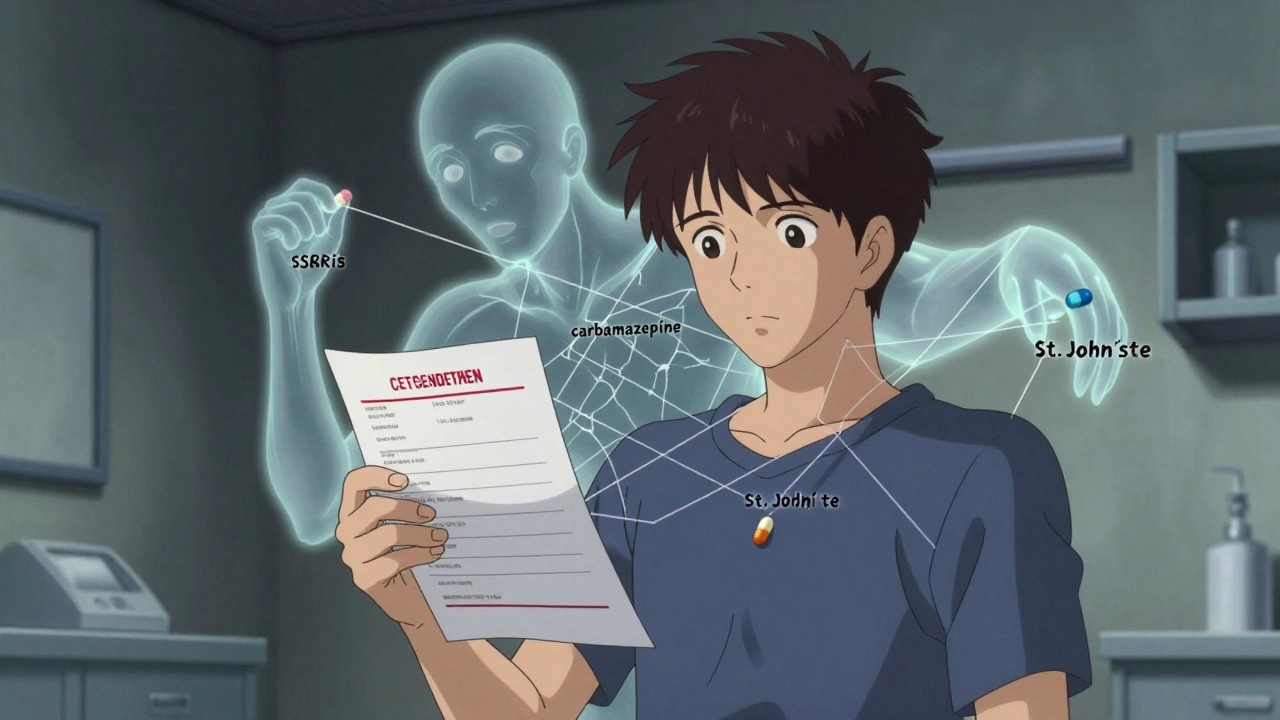
Psychiatric Meds: The Hidden Wild Card
Transgender people are more likely to experience depression, anxiety, and PTSD. Many take SSRIs like fluoxetine (Prozac) or sertraline (Zoloft). These can interact with GAHT-but not how you’d think.
SSRIs like fluoxetine block CYP2D6, another liver enzyme. That enzyme helps break down estradiol. So if you’re on fluoxetine, your estrogen levels might rise slightly. Not enough to cause alarm, but enough that you might notice more breast tenderness or mood changes.
The bigger issue? Testosterone can reduce the effectiveness of some antidepressants. A 2023 review found 17 cases where people on testosterone suddenly felt their depression returning. Their SSRI dose was unchanged, but their body was processing it differently. In every case, increasing the SSRI dose by 25-50% helped.
Then there are mood stabilizers. Carbamazepine (Tegretol), used for bipolar disorder or seizures, is a strong CYP3A4 inducer. It can slash estrogen levels by up to 40%. If you’re on this drug, your provider may need to raise your estradiol dose-or switch you to a non-interacting mood stabilizer like lamotrigine.
The scary part? Most antidepressant trials never included transgender people. So we’re guessing a lot of the time. That’s why monitoring your mood, energy, and sleep isn’t optional-it’s essential.
Other Common Medications to Watch For
Here’s a quick cheat sheet for drugs that might mess with GAHT:
- Antibiotics: Rifampin (used for TB) is a strong CYP3A4 inducer. Avoid it if you’re on estrogen. If you must take it, expect to need higher estradiol doses.
- Seizure meds: Phenobarbital, phenytoin, and topiramate can all lower hormone levels. Monitor closely.
- St. John’s Wort: This herbal supplement is a powerful CYP3A4 inducer. It can cut estrogen levels by half. Don’t take it while on GAHT.
- Blood thinners: Estradiol increases clotting risk. If you’re on warfarin or apixaban, your provider may need to adjust your dose more often.
- Thyroid meds: Estrogen can raise thyroid-binding proteins, making your T4 levels look high on blood tests-even if you’re not overmedicated. Your doctor should check free T4 and TSH, not total T4.

What You Should Do Right Now
Don’t wait for a crisis. Here’s what to do today:
- Make a full list of every medication you take-including supplements, OTC painkillers, and herbal products.
- Bring it to your endocrinologist or primary care provider and ask: "Which of these could affect my hormones?" Don’t assume they know.
- Ask for hormone level checks before and 4-6 weeks after starting or changing any new medication.
- Track your symptoms-mood, energy, breast tenderness, acne, headaches. Write them down. Patterns matter more than single numbers.
- Don’t stop or change your meds on your own. Even if you think something’s causing a problem, talk to your provider first.
Many clinics still don’t have standardized screening for these interactions. A 2023 audit found only 41% of U.S. endocrinology clinics routinely check for drug-hormone conflicts. That means you might be the only one watching out for you.
What’s Changing in 2025
The field is moving fast. The NIH is running the Tangerine Study, tracking how 300 transgender adults respond to 12 common psychiatric drugs while on GAHT. Results will be out in mid-2025. That’s the first large-scale data we’ve ever had.
Drug companies are finally starting to test new meds in transgender people. Gilead, maker of PrEP, now requires GAHT interaction studies in all future trials. That’s a big step.
But gaps remain. We still don’t know how newer drugs like brexanolone (for postpartum depression) or long-acting cabotegravir interact with GAHT. There are only two case reports on these combinations-and both were published in 2023.
For now, the safest rule is this: if it’s new, be cautious. If it affects your liver, your mood, or your hormones, ask questions. And don’t let anyone tell you that your needs are too niche to matter. You’re not an afterthought. You’re the reason this research exists.
Final Thought: You’re Not Alone in This
Gender-affirming care is personal. But it’s also medical. And like any medical treatment, it works best when you’re informed. You don’t need to be a scientist. You just need to know what to ask for. Keep your list of meds handy. Track your body’s signals. Speak up when something feels off. Your hormones are powerful-but they’re not magic. They respond to the world around them. And with the right knowledge, you can make sure that world supports you, not works against you.

Sangram Lavte
Just wanted to say this is one of the clearest breakdowns I’ve read on GAHT interactions. The CYP3A4 explanation alone saved me from a bad med switch last year. If you’re on anything beyond hormones, get your liver enzymes checked quarterly.
Nicholas Heer
THEY DON’T WANT YOU TO KNOW THIS BUT THE PHARMA COMPANIES ARE HIDING THE TRUTH ABOUT ESTROGEN AND HIV DRUGS. THEY’RE USING CYP3A4 TO CONTROL YOUR BODY AND KEEP YOU DEPENDENT. THE NIH ISN’T STUDYING THIS BECAUSE THEY’RE PAID OFF. I SAW A WHISPERED DOCUMENT ON 4CHAN THAT SHOWED THEY’RE INVESTING IN A NEW DRUG THAT MAKES TRANS PEOPLE NEED HIGHER DOSES. THEY WANT YOU SICK.
Ernie Blevins
So you’re telling me taking testosterone makes SSRIs less effective? Wow. That’s wild. I guess that’s why I felt like crap after starting HRT. Should’ve just stayed on meds and not bothered.
Oliver Damon
This is a critical piece. The CYP enzyme dynamics aren’t just pharmacological-they’re existential. When your body’s metabolic pathways are hijacked by polypharmacy, you’re not just adjusting doses-you’re renegotiating your biological autonomy. The fact that 41% of clinics don’t screen for this isn’t negligence-it’s systemic epistemic violence. We need standardized pharmacogenomic panels for trans patients, not just reactive symptom management.
Kurt Russell
LISTEN UP. IF YOU’RE ON GAHT AND YOU’RE NOT TRACKING YOUR MOOD, YOUR BREAST TENDERNESS, OR YOUR SLEEP-YOU’RE PLAYING RUSSIAN ROULETTE WITH YOUR BODY. I WAS ON 80MG OF TESTO GEL AND STARTED TOPAMAX FOR MIGRAINES. MY TESTOSTERONE DROPPED LIKE A ROCK. I THOUGHT I WAS DEPRESSED. TURNED OUT I WAS JUST LOW ON HORMONES. GOT MY DOSE ADJUSTED. LIFE CHANGED. DON’T BE A STATISTIC. KNOW YOUR MEDS.
Wesley Phillips
PrEP doesn't interfere? Lmao. You really believe that? Everyone knows tenofovir suppresses testosterone absorption. The study was funded by Gilead. They just want you to keep buying pills. I’ve been on Truvada for 3 years and my T levels are trash. They just don’t tell you that part.
Desmond Khoo
THIS IS SO IMPORTANT!! 🙌 I just switched from efavirenz to dolutegravir and my estrogen levels stabilized in 2 weeks. I cried. I actually cried. You guys are doing god’s work putting this out there. Thank you. I’m sharing this with my whole trans support group. 💪❤️
Louis Llaine
Wow. A whole article about how to not die from your own hormones. Groundbreaking. Next up: 'How to Not Fall Off a Ladder While Climbing It.' Maybe we can get a PhD in Common Sense.
Jane Quitain
i just started spironolactone and i think my anxiety got worse? i dont know if its the med or me or if im just being dramatic but i keep checking my blood pressure and i think i might be having a stroke??
Stacy here
Let’s be real-this isn’t about drug interactions. It’s about control. Who gets to decide what your body is allowed to become? The FDA? Big Pharma? Your doctor who hasn’t read a trans health paper since 2015? They want you docile. They want you silent. They want you to take your pills and never question why your estrogen dose changed after you got a new insurance plan. This article is a spark. Don’t let them snuff it out. Fight for your chemistry. Fight for your right to metabolize freely. Your body is not a lab rat.
Sam Mathew Cheriyan
Wait so st johns wort is bad? lol i thought it was natural so it was safe. guess i was wrong again. but what about that guy on reddit who said he took it for 2 years and his boobs got bigger? maybe the study is fake? maybe the cyp3a4 thing is just a scam? i think the government made up the enzyme thing to sell more meds.