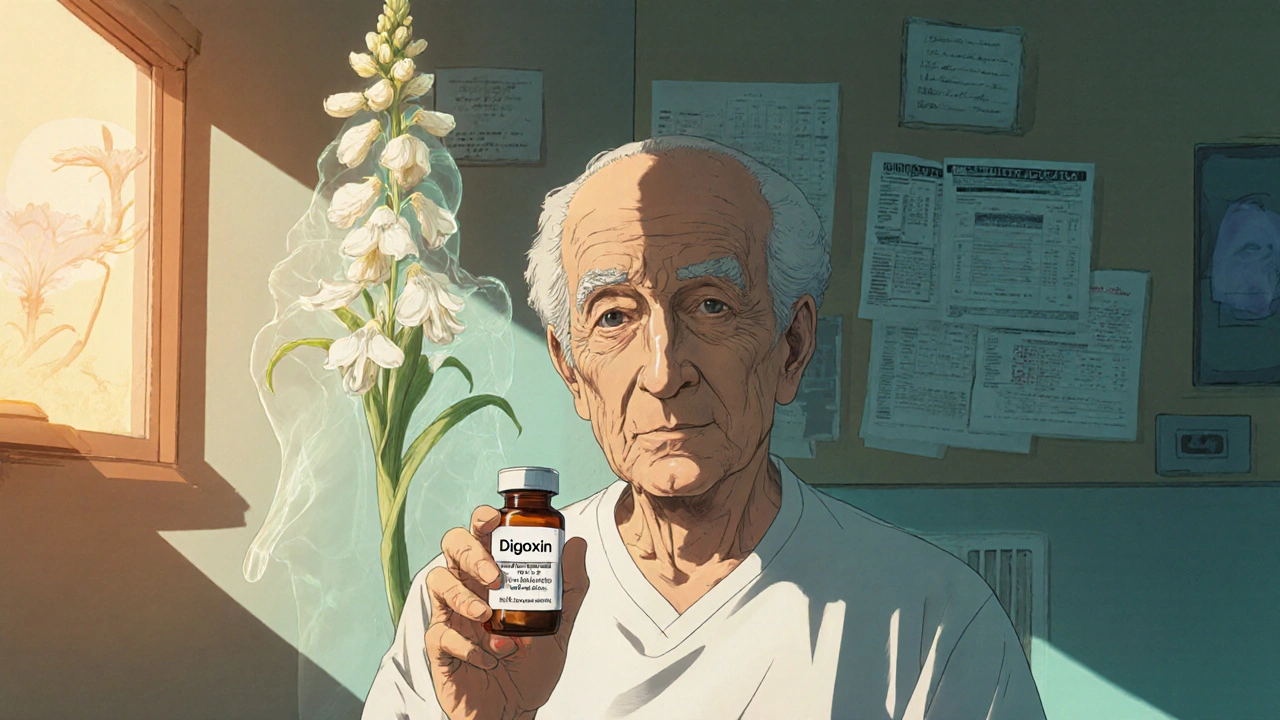
Digoxin has been used for over 200 years to treat heart failure and atrial fibrillation. It’s not new, but it’s still prescribed - especially when other drugs don’t work or aren’t tolerated. Yet many patients and even some doctors wonder: is there something better? With newer medications available, the role of digoxin has shifted. This isn’t about ditching an old drug. It’s about knowing when it helps, when it doesn’t, and what else you can try.
How Digoxin Actually Works
Digoxin comes from the foxglove plant. It slows down the heart rate and makes each heartbeat stronger. That’s useful in two situations: when your heart beats too fast and irregularly (like in atrial fibrillation), or when it’s too weak to pump blood well (heart failure).
It doesn’t cure anything. It doesn’t extend life like some newer drugs. But it does help people feel better - less short of breath, less tired. Studies show it reduces hospital visits for heart failure by about 20%. That matters. For someone who’s been in and out of the hospital, fewer trips mean better quality of life.
But here’s the catch: digoxin has a tiny window between working and poisoning. The difference between a good dose and a dangerous one is small. Blood levels must be checked regularly. Even minor changes in kidney function or other meds can push it into toxic territory.
Why Doctors Still Prescribe It
Digoxin isn’t first-line anymore. Guidelines from the American Heart Association and European Society of Cardiology now recommend beta-blockers, ACE inhibitors, ARBs, SGLT2 inhibitors, and mineralocorticoid receptor antagonists before digoxin.
So why use it at all?
- When heart rate control with beta-blockers or calcium channel blockers isn’t enough
- When patients can’t tolerate other drugs due to low blood pressure or slow heart rate
- When someone has persistent atrial fibrillation and isn’t a candidate for rhythm control
- When cost is a major factor - digoxin costs less than $10 a month in the U.S.
It’s often added on top of other meds, not used alone. Think of it like a backup singer - not the lead, but it fills in the gaps.
Top Alternatives to Digoxin
There’s no single replacement for digoxin. But several drugs do similar jobs - and often better.
1. Beta-Blockers: Metoprolol, Carvedilol, Bisoprolol
These are the first choice for controlling heart rate in atrial fibrillation and improving survival in heart failure. They slow the heart, reduce oxygen demand, and protect the heart muscle.
Compared to digoxin:
- They lower death risk by 30-35% in heart failure
- They’re safer - less risk of toxicity
- They work better for exercise tolerance
Downside? They can make you tired, lower blood pressure too much, or worsen asthma. Not everyone can take them.
2. Calcium Channel Blockers: Diltiazem, Verapamil
Good for rate control in atrial fibrillation, especially if beta-blockers aren’t enough. They work fast and are often used in younger patients or those with high blood pressure.
But they’re not for everyone:
- Avoid if you have severe heart failure - they can make pumping worse
- Can cause dizziness or constipation
- Not recommended with digoxin - they increase digoxin levels and raise toxicity risk
3. SGLT2 Inhibitors: Empagliflozin, Dapagliflozin
These were originally diabetes drugs. Now they’re a game-changer for heart failure - even in people without diabetes.
They reduce hospitalizations by 30% and lower death risk by 20-25%. They also help with fluid buildup, weight loss, and kidney protection.
Compared to digoxin:
- They improve survival - digoxin doesn’t
- They’re taken once daily, no blood tests needed
- Side effects? Minor: increased urination, occasional yeast infections
They’re now recommended before digoxin in most cases.
4. ARNI: Sacubitril/Valsartan (Entresto)
This combo drug replaces ACE inhibitors or ARBs in patients with reduced ejection fraction (a sign of weak heart pumping).
It cuts heart failure hospitalizations by 21% and reduces death by 20% compared to enalapril. It’s not for rate control, but it’s a powerful tool for improving heart function.
Digoxin can still be added if symptoms persist, but ARNI is now the backbone of treatment.
5. Antiarrhythmics: Amiodarone, Dronedarone, Flecainide
If the goal is to restore normal heart rhythm (not just slow it), these drugs are better than digoxin.
Amiodarone is strong but has serious long-term side effects - lung, thyroid, liver damage. Dronedarone is safer but less effective. Flecainide works well in people without structural heart disease.
Digoxin doesn’t restore rhythm. It just slows the heart. If rhythm control is the goal, these are the right tools.

Digoxin vs Alternatives: Quick Comparison
| Drug | Primary Use | Survival Benefit | Requires Blood Monitoring | Cost (Monthly) | Key Side Effects |
|---|---|---|---|---|---|
| Digoxin Cardiac glycoside used for rate control in atrial fibrillation and symptom relief in heart failure | Rate control, symptom relief | No | Yes | $5-$15 | Nausea, vision changes, arrhythmias, toxicity |
| Metoprolol Beta-blocker for heart rate control and heart failure management | Rate control, survival improvement | Yes (30-35% reduction) | No | $10-$20 | Fatigue, low BP, cold hands, bronchospasm |
| Dapagliflozin SGLT2 inhibitor for heart failure with reduced ejection fraction | Heart failure, reduces hospitalizations | Yes (20-25% reduction) | No | $150-$200* | Urination, yeast infections, dehydration risk |
| Sacubitril/Valsartan ARNI for heart failure with reduced ejection fraction | Improves heart function, reduces hospitalizations | Yes (20% reduction) | No | $500-$700* | Low BP, kidney changes, angioedema |
| Diltiazem Calcium channel blocker for atrial fibrillation rate control | Rate control | No | No | $15-$30 | Dizziness, constipation, swelling |
*Costs vary by insurance. Generic versions of dapagliflozin are now available and cost less than $10/month in some plans.
Who Should Avoid Digoxin
Digoxin isn’t safe for everyone. Avoid it if you have:
- Severe kidney disease - digoxin is cleared by the kidneys. Poor function = toxic buildup
- Heart block without a pacemaker - it can make slow heart rhythms worse
- Low potassium or magnesium - these imbalances increase toxicity risk
- History of digoxin toxicity - once you’ve had it, you’re more likely to get it again
- Interactions with common drugs: amiodarone, quinidine, verapamil, cyclosporine, macrolide antibiotics
Even healthy people need monitoring. A simple blood test every 6-12 months can prevent disaster.
When to Stick With Digoxin
There are real cases where digoxin still makes sense:
- Older adults with persistent atrial fibrillation who can’t tolerate beta-blockers
- Patients with advanced heart failure who still feel tired despite other meds
- Those without insurance who can’t afford newer drugs - digoxin is the most affordable option
- People who’ve been on it for years with no issues and feel fine
Don’t stop digoxin just because it’s old. If it’s working and safe, keep it. But always ask: could something better be added?
What You Should Ask Your Doctor
If you’re on digoxin, here are five questions to ask at your next visit:
- Is my digoxin level checked regularly? What’s my current level?
- Have I been evaluated for SGLT2 inhibitors or ARNI? Would they help me more?
- Am I on the lowest effective dose? Could I lower it?
- Do I have any signs of toxicity - nausea, blurry yellow vision, dizziness?
- Are there any new drugs I should consider that might reduce hospital visits or improve survival?
These aren’t hard questions. They’re smart ones. Doctors appreciate patients who ask.
Bottom Line
Digoxin isn’t dead. But it’s no longer the star. It’s a supporting player - useful in specific cases, especially when other options aren’t possible. Newer drugs like SGLT2 inhibitors and ARNI do more: they save lives, reduce hospital stays, and work without constant monitoring.
If you’re on digoxin and doing well, that’s good. But don’t assume it’s the best you can do. Ask about alternatives. Ask about blood tests. Ask about your goals - do you want to feel better, or do you want to live longer? The answer should guide your treatment.
Heart disease treatment has changed. Digoxin still has a place - but it’s no longer the only one.
Is digoxin still used today?
Yes, but less often than before. Digoxin is still prescribed for atrial fibrillation when heart rate control is hard to achieve with beta-blockers or calcium channel blockers, and for heart failure patients who still have symptoms despite modern treatments. It’s mainly used as an add-on therapy now, not a first choice.
What are the dangers of digoxin?
The biggest danger is toxicity, which can happen even at normal doses if kidney function drops or if other drugs interact with it. Signs include nausea, vomiting, confusion, vision changes (like yellow or blurred vision), and irregular heartbeats. Toxicity can be life-threatening. Regular blood tests are essential.
Can I take digoxin with other heart meds?
Some are safe, others are risky. Digoxin interacts badly with amiodarone, verapamil, diltiazem, quinidine, and certain antibiotics like clarithromycin. These can raise digoxin levels and cause toxicity. Always tell your doctor and pharmacist about every medication you take - including supplements and over-the-counter drugs.
Are there natural alternatives to digoxin?
No. While some herbal supplements like hawthorn or coenzyme Q10 are promoted for heart health, none have proven effects on heart rate or survival like digoxin or modern drugs. Natural doesn’t mean safe or effective. Relying on herbs instead of prescribed treatment can be dangerous.
Why is digoxin cheaper than other heart meds?
Digoxin is an old drug, off-patent for decades. Generic versions are mass-produced and sold at low margins. Newer drugs like SGLT2 inhibitors and ARNI are still under patent or have complex manufacturing, so they cost more. Price doesn’t mean better - but cost matters when you’re paying out of pocket.
Can I stop digoxin if I start a new medication?
Maybe - but never on your own. If you start an SGLT2 inhibitor or ARNI and feel better, your doctor might reduce or stop digoxin. But stopping suddenly can cause rebound symptoms. Always follow your doctor’s plan for tapering or switching.
Does digoxin help with atrial fibrillation symptoms?
Yes, it helps control the heart rate, which reduces palpitations, shortness of breath, and fatigue in many people. But it doesn’t restore normal rhythm. If you’re still feeling symptoms, your doctor may need to add another drug or consider rhythm control options like ablation.
How often should digoxin levels be checked?
Typically every 6 to 12 months if you’re stable. But more often if you’re sick, start new meds, have kidney problems, or show signs of toxicity. Some doctors check after starting or changing the dose, then every 2-4 weeks until levels are steady.
Next Steps
If you’re on digoxin:
- Ask your doctor for your current digoxin blood level - write it down
- Review all your medications with your pharmacist - look for interactions
- Ask if you’re a candidate for SGLT2 inhibitors or ARNI - especially if you have heart failure
- Monitor for symptoms of toxicity: nausea, vision changes, irregular heartbeat
- Don’t skip kidney function tests - they’re just as important as digoxin levels
If you’re not on digoxin but have atrial fibrillation or heart failure:
- Ask if newer drugs like dapagliflozin or sacubitril/valsartan are right for you
- Understand that treatment goals have changed - it’s not just about rate control anymore
- Ask what your long-term plan is - do you need to live longer, or just feel better?
Heart disease treatment isn’t static. The best choice today might not be the best next year. Stay informed. Stay involved. Your health is worth it.
Rachel Puno
digoxin is literally ancient history like why are we still talking about this drug like its 1987 🤡
Brad Seymour
i get it digoxin is cheap and works for some folks but honestly if you're still on it without trying an SGLT2 inhibitor you're basically leaving money on the table. my uncle was on digoxin for years then switched to dapagliflozin and his ejection fraction jumped 15% in 6 months. no blood tests no drama just better living. why not ask your doc?
Malia Blom
people treat digoxin like its some evil relic but its just a tool like a hammer. if your house is falling apart you don't throw out the hammer because someone invented a nail gun. sometimes the old thing still works better than the shiny new thing that costs 500 bucks a month. also i think we're all forgetting that medicine isn't about being trendy its about what keeps you alive and not in the hospital. and digoxin does that for a lot of people who can't afford the latest hype pills
Erika Puhan
the data is unequivocal. digoxin has no mortality benefit. period. sgl2 inhibitors demonstrate statistically significant reduction in all-cause mortality and hf hospitalizations. the aha/esc guidelines are clear. continuing digoxin as monotherapy or even as adjunct without sglt2i is a deviation from evidence-based practice. if your clinician is still prescribing it as first-line you're being managed by a relic of the 20th century. also your renal clearance kinetics are probably suboptimal. get a gfr.
Edward Weaver
usa has the best healthcare in the world and we're still using this 200 year old drug because some people can't afford the $200 pill? that's not medicine thats capitalism. if you can't afford dapagliflozin then your system is broken not your meds. digoxin is a bandaid on a bullet wound. we need universal healthcare not cheaper poisons.
Lexi Brinkley
my grandma has been on digoxin since 1998 and she still gardens every morning 🌷 no hospital visits in 5 years. if it ain't broke don't fix it! 💪❤️
Rachel Puno
so you're saying we should keep giving people poison because grandma likes it? 🤦♂️
Kelsey Veg
i think u guys are overcomplicating this. digoxin works for some ppl. sgl2i works for others. its not one size fits all. also the cost thing is real. i know people who literally choose between food and meds. if digoxin keeps them alive and out of the er then why are we acting like its evil? its not the drug its the system.
Alex Harrison
i been on digoxin since 2018 and my levels are always in range. my doc checks em every 6 months. i feel better than i did on beta blockers. i dont care if its old if it works. also i dont wanna pay 500 a month for a pill that makes me pee all day. just sayin.