Varicose Veins: Understanding, Treating, and Preventing This Common Condition
When dealing with varicose veins, enlarged, twisted veins that usually appear on the legs and cause discomfort or cosmetic concerns. Also known as spider veins, they are a hallmark of chronic venous insufficiency, a condition where vein walls and valves fail to return blood efficiently to the heart. The most effective first line of defense often involves compression therapy, which uses specially designed stockings to apply graduated pressure and improve circulation. For stubborn cases, sclerotherapy offers a minimally invasive option that injects a solution to close off the faulty veins. These three entities—varicose veins, chronic venous insufficiency, and compression therapy—form a tight loop where each influences the other, creating a clear pathway for management.
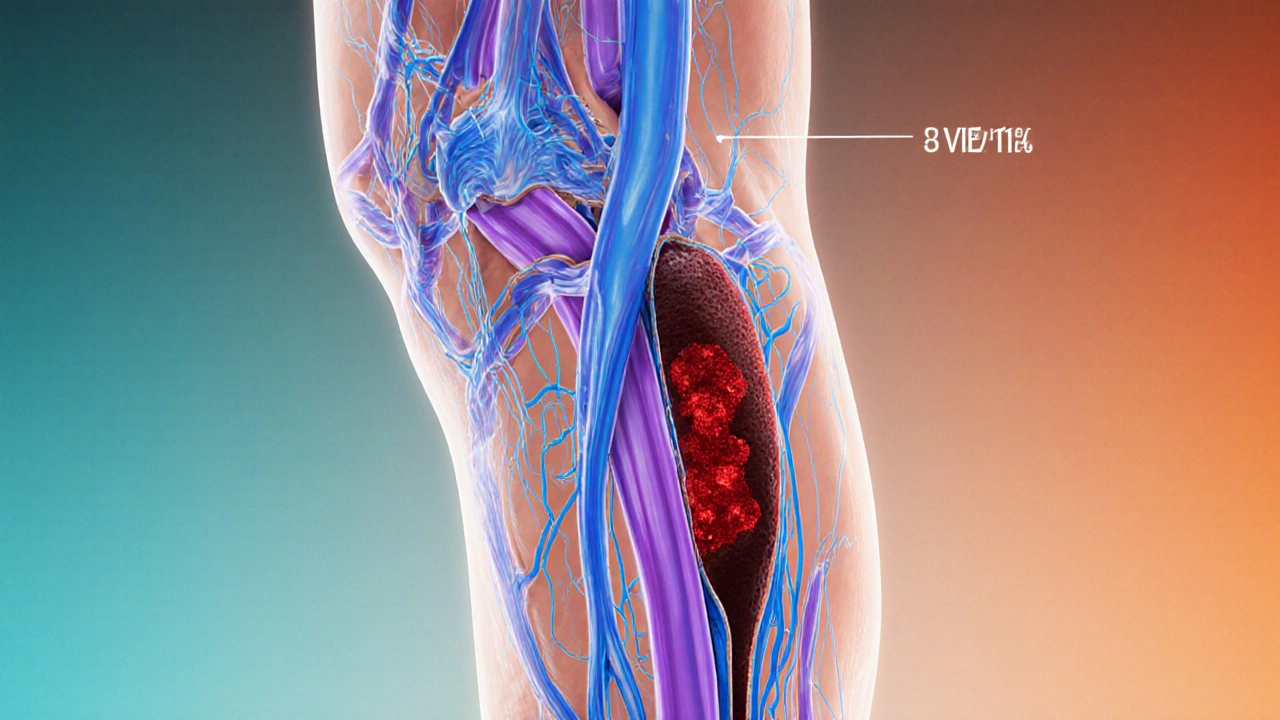
Varicose veins often start with weakened vein walls, which leads to blood pooling and increased pressure. This pressure triggers the formation of visible, bulging veins—a classic symptom of chronic venous insufficiency. Lifestyle factors such as prolonged standing, obesity, and pregnancy can exacerbate the problem by raising venous pressure. Understanding this cause‑effect chain helps you spot early signs and act before the veins become painful or ulcerated.
Key Treatment Paths and When to Choose Them
The first step for most patients is to try compression therapy. Properly fitted stockings apply about 15‑20 mmHg at the ankle, decreasing as they rise toward the thigh. This pressure forces blood back toward the heart, reducing swelling and preventing new vein damage. If compression alone isn’t enough, doctors may recommend sclerotherapy, especially for smaller varicose or spider veins. The procedure involves injecting a sclerosant that irritates the vein lining, causing it to collapse and fade over weeks. For larger, bulging veins, laser or radiofrequency ablation can seal the vein off, while surgical vein stripping remains a fallback for complex cases.
Each treatment choice comes with its own set of pros and cons. Compression therapy is low‑cost, non‑invasive, and can be used long‑term, but it requires consistent wear and proper sizing. Sclerotherapy offers quick cosmetic results with minimal downtime, yet multiple sessions may be needed and it isn’t ideal for veins larger than a few millimeters. Surgical options provide permanent removal but carry higher risks of infection and longer recovery. Knowing these trade‑offs lets you align the method with your lifestyle, pain tolerance, and budget.
Beyond medical interventions, daily habits play a huge role in keeping veins healthy. Elevating your legs above heart level for a few minutes each day reduces pressure and speeds fluid return. Regular low‑impact exercise—like walking, swimming, or cycling—strengthens calf muscles, which act as a natural pump for leg veins. Wearing loose‑fitting clothing and avoiding tight socks or belts also helps maintain healthy circulation.
Nutrition can subtly influence vein health too. Foods rich in flavonoids—such as berries, citrus fruits, and leafy greens—support vein wall integrity. Limiting salt intake reduces fluid retention, lessening swelling in the lower legs. Staying hydrated maintains optimal blood volume, making it easier for the circulatory system to function smoothly.
When evaluating treatment options, it’s useful to consider three semantic triples that capture the core relationships: (1) Varicose veins are a symptom of chronic venous insufficiency; (2) Compression therapy helps manage varicose veins by improving blood flow; (3) Sclerotherapy can resolve visible varicose veins by closing the faulty vessels. These connections illustrate how diagnosis, lifestyle, and treatment intertwine.
If you notice pain, swelling, skin changes, or ulcers around your ankles, seek medical advice promptly. Early intervention can prevent complications like deep vein thrombosis or chronic ulcers. A vascular specialist can assess vein function with Doppler ultrasound, determine the severity of insufficiency, and recommend the most suitable therapy.
In summary, understanding the causes, recognizing the signs, and choosing the right combination of compression, minimally invasive procedures, or surgery empowers you to take control of varicose veins. The next section below showcases a range of articles—from medication guides to lifestyle tips—that complement this overview and help you make informed decisions about your vascular health.
Deep Vein Thrombosis and Varicose Veins: How They're Linked and What to Do
Explore how varicose veins and deep vein thrombosis are connected, learn shared risk factors, symptoms to watch for, and practical steps to prevent serious complications.