DVT and Varicose Veins Risk Calculator
Your Risk Factors
Select the factors that apply to you to calculate your risk level.
Risk Level
Select your risk factors to see your risk level
About This Calculator
This tool estimates your risk of developing either DVT or varicose veins based on key risk factors. It's designed for educational purposes and should not replace professional medical advice.
Remember: Most people with varicose veins do not develop DVT, but shared risk factors make awareness important.
Quick Takeaways
- Varicose veins can increase the odds of developing deep vein thrombosis, but the risk is still relatively low for most people.
- Both conditions share common risk factors such as inactivity, obesity, and genetics.
- Early signs-pain, swelling, or a sudden change in a leg’s appearance-should prompt medical evaluation.
- Diagnosis usually involves ultrasound imaging, and treatment ranges from compression therapy to anticoagulant medication.
- Lifestyle tweaks-regular movement, weight control, and proper footwear-help prevent both problems.
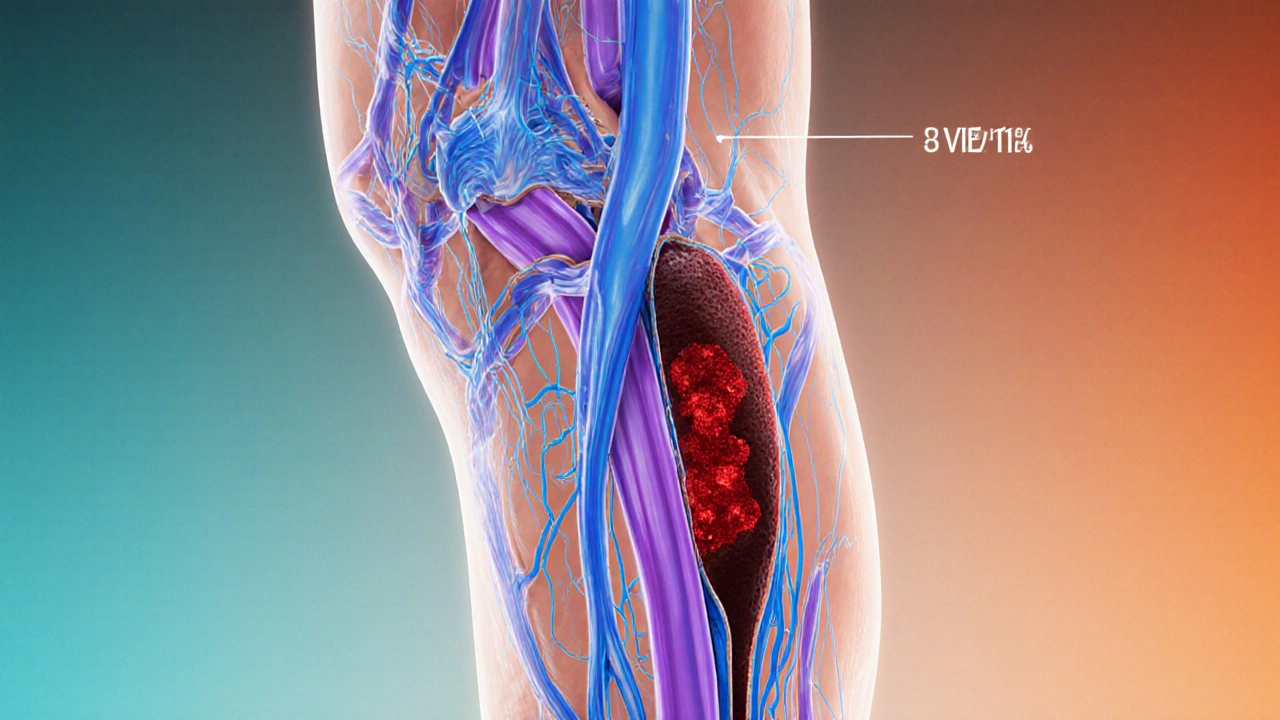
What Is Deep Vein Thrombosis?
Deep Vein Thrombosis is a condition where a blood clot forms in the deep veins, most often in the thighs or calves. The clot can partially or completely block blood flow, causing swelling, pain, and in severe cases, can dislodge and travel to the lungs, leading to a pulmonary embolism. According to a 2023 epidemiology report, about 1 in 1,000 adults will experience a DVT each year, making it a leading cause of preventable hospital admissions.
What Are Varicose Veins?
Varicose veins are enlarged, twisted superficial veins that usually appear on the lower legs. They result from faulty venous valves, which allow blood to pool and increase pressure in the vein wall. While largely cosmetic, varicose veins can cause heaviness, aching, and, in some cases, skin changes or ulcers.

How the Two Conditions Are Linked
Both DVT and varicose veins involve problems with blood flow in the legs, but they affect different parts of the venous system. The link comes from several physiological pathways:
- Venous stasis: When valves in superficial veins fail (as in varicose veins), blood can back up, increasing pressure in deeper veins and slowing circulation-an environment where clots like to form.
- Inflammation: Dilated veins release inflammatory mediators that can make the inner lining of deep veins more prone to clotting.
- Shared risk factors: Obesity, prolonged sitting, pregnancy, and genetic clotting disorders raise the odds for both conditions.
Even though the overlap exists, most people with varicose veins never develop a DVT. The actual added risk varies, with studies estimating a 1.5‑ to 2‑fold increase compared to peers without varicose veins.
Common Risk Factors
Understanding what drives both problems helps you target prevention. Below are the biggest culprits:
- Age - risk rises sharply after 50.
- Genetics - a family history of clotting disorders (e.g., Factor V Leiden) or varicose veins amplifies risk.
- Obesity - excess weight puts extra pressure on leg veins.
- Prolonged immobility - long flights, desk jobs, or recovery from surgery.
- Hormonal changes - pregnancy, oral contraceptives, and hormone replacement therapy.
When to Seek Medical Attention
Both conditions can be silent until something changes. Watch for these red‑flag symptoms:
- Sudden, intense calf or thigh pain that doesn’t ease with rest.
- Swelling that appears quickly-especially if one leg looks larger than the other.
- Warmth, redness, or tenderness over a vein.
- Shortness of breath, chest pain, or rapid heartbeat (possible sign of pulmonary embolism).
If any of these appear, call your healthcare provider or go to the ER right away. Early treatment reduces the chance of serious complications.
How Doctors Diagnose the Problem
Diagnosis usually starts with a physical exam, but imaging is essential for confirming a clot or assessing vein health.
- Doppler ultrasound - non‑invasive, shows blood flow and can detect clots in deep veins.
- Compression ultrasound - evaluates valve function in superficial veins for varicose veins.
- Blood tests - D‑dimer levels can suggest clot presence, while genetic panels identify inherited clotting disorders.

Treatment Options and Prevention Strategies
Management differs depending on whether you have a clot, varicose veins, or both.
| Aspect | Deep Vein Thrombosis | Varicose Veins |
|---|---|---|
| Primary concern | Blood clot, risk of pulmonary embolism | Cosmetic appearance, discomfort, skin changes |
| Typical treatment | Anticoagulants, possible thrombolysis | Compression stockings, sclerotherapy, laser ablation |
| Urgency | Medical emergency if embolism suspected | Usually elective, unless complications develop |
| Diagnostic tool | Doppler ultrasound | Duplex ultrasound, physical exam |
For DVT, the cornerstone is anticoagulation. Options include warfarin, direct oral anticoagulants (DOACs) like apixaban, and, in severe cases, catheter‑directed thrombolysis. Therapy typically lasts three to six months, with follow‑up blood monitoring.
Varicose veins are managed first with lifestyle changes and graduated compression stockings-preferably compression stockings that exert 15‑20 mmHg pressure. If symptoms persist, minimally invasive procedures such as endovenous laser therapy, radiofrequency ablation, or ultrasound‑guided sclerotherapy provide lasting relief.
Everyday Habits That Lower the Risk
Even if you already have varicose veins, simple daily moves can keep clots at bay:
- Take a 5‑minute walk every hour-especially on long trips.
- Do ankle pumps and calf raises while seated to promote venous return.
- Stay hydrated; dehydration thickens blood.
- Maintain a healthy weight through balanced diet and regular exercise.
- Avoid tight clothing that compresses the thigh or groin area.
For those at higher risk-people with a known clotting disorder, recent surgery, or a strong family history-your doctor may recommend a short course of prophylactic anticoagulation after major procedures.
When to See a Specialist
If you’ve been diagnosed with varicose veins and notice any of the following, book an appointment with a vascular specialist:
- Rapid swelling or new pain that wasn’t there before.
- Skin discoloration, ulceration, or bleeding from a vein.
- History of a previous DVT or pulmonary embolism.
Specialists can run a comprehensive duplex scan, assess your overall vein health, and tailor a treatment plan-whether that means a more aggressive compression regimen or an interventional procedure.
Frequently Asked Questions
Can varicose veins cause a blood clot?
Yes, they can increase the risk because poor valve function leads to blood pooling, which creates a favorable environment for clot formation. However, most people with varicose veins never develop a clot.
How is DVT different from a superficial vein thrombosis?
DVT occurs in deep veins and can lead to a pulmonary embolism, while superficial thrombosis involves veins just under the skin and is usually less dangerous.
Do compression stockings prevent DVT?
They help reduce stasis and are recommended during long travel or after surgery, but they are not a substitute for anticoagulant medication when a clot is already present.
Is surgery the only cure for varicose veins?
No. Many patients improve with compression, lifestyle changes, and minimally invasive procedures like laser ablation, which have shorter recovery times than traditional vein stripping.
What tests confirm a pulmonary embolism?
CT pulmonary angiography is the gold standard, often preceded by a D‑dimer blood test and a clinical risk assessment.
Amanda Jennings
Hey folks, if you’re curious about how your lifestyle tweaks impact DVT and varicose veins, give this calculator a spin. Even a quick check can spotlight hidden habits that need a tweak, like moving more during those long work days. Keep the momentum going – a little awareness now can keep the veins happy later.
alex cristobal roque
Alright, let’s break down why those risk factors matter and what you can actually do about them. Age over 65 bumps your baseline risk because the venous walls naturally lose elasticity, making clots more likely to form. A family history of DVT or varicose veins injects a genetic component, so you’re essentially inheriting a predisposition to weaker valve function. Carrying extra weight adds pressure to the lower extremities, which can aggravate venous pooling and set the stage for thrombosis. Sedentary habits, especially those marathon sitting sessions, reduce the muscle pump that normally helps push blood back toward the heart. Hormonal influences like oral contraceptives or hormone replacement therapy increase clotting factors in the blood, so they’re a notable red flag. Recent surgeries, even minor orthopedic procedures, often involve periods of immobilization that let blood stagnate. All these pieces get tallied by the calculator, giving you a composite risk score that’s more than just a number – it’s a call to action. If the score lands in the higher tier, the next step is to schedule a chat with your primary care physician or a vascular specialist. They can run duplex ultrasounds or coagulation panels to rule out hidden issues. In the meantime, crank up your daily steps, aim for at least 7,000 to 10,000, and incorporate calf raises during TV commercials. Hydration also plays a silent role; staying well‑watered keeps blood viscosity in check. If you’re on hormonal therapy, discuss alternatives with your doctor, especially if you have other risk factors. Compression stockings aren’t just for aesthetics; they provide graduated pressure that helps the veins push blood upward. And remember, smoking cessation is a powerhouse move – nicotine constricts vessels and spikes clotting potential. Lastly, keep an eye on any new leg swelling, pain, or discoloration; early detection can prevent a full‑blown DVT. Use the calculator as a baseline, not a verdict, and keep tweaking those lifestyle variables for a healthier vascular future.
Bridget Dunning
Colleagues, the interrelationship between deep vein thrombosis and varicose venous pathology hinges upon shared etiological vectors, notably venous hypertension and endothelial dysfunction. In physiologic terms, valve incompetence precipitates retrograde flow, engorging superficial tributaries and fostering varicosities, while the resultant stasis constitutes a pivotal element of Virchow’s triad for thrombogenesis. Genetic polymorphisms in coagulation cascade genes further exacerbate susceptibility, thereby underscoring the merit of a comprehensive risk assessment. The calculator delineated herein aptly stratifies these variables, yet it remains a pedagogic adjunct rather than a substitute for duplex ultrasonography. Clinical vigilance is advised when patients present with edema, cutaneous discoloration, or disproportionate pain, as these may herald an incipient thrombus. Preventative strategies should integrate graduated compression therapy, optimized body mass index, and judicious pharmacologic modulation where indicated. I commend the developers for synthesizing a user‑centric interface that facilitates shared decision‑making between clinicians and laypersons.
Shweta Dandekar
Honestly, if you aren't moving, you're practically inviting a clot!!!
Gary Smith
Look, America has the best medical research, the best hospitals, and we shouldn't settle for vague calculators that just spit out numbers, you need a real doctor, a real plan, and a real commitment to staying healthy, not some generic tool that pretends to care about our veins.
Dominic Dale
They don’t want you to realize that the pharmaceutical giants are quietly funding these risk calculators to push unnecessary medication. You see the pattern every time a new “tool” appears, it’s followed by a surge in prescription anticoagulants. The data they present is cherry‑picked, the real agenda is profit, not patient well‑being. While the calculator mentions compression stockings, you’ll never hear about the lucrative market for branded compression garments. The “educational purposes” disclaimer is a thin veil for commercial exploitation. So stay skeptical and demand transparency before you trust any online risk assessment.
christopher werner
I appreciate the thorough rundown; staying informed is the first step toward prevention.
Matthew Holmes
The veins whisper warnings in every ache, you feel it before you understand it The risk calculator is just a flicker in a storm of blood
Patrick Price
Yo the veiinss calculator is kinda cool but i saw a typo in the weight status dropdown it says “obes” instead of “obese” also the calcualtor sometimes freezes when i click calculate can u fix?
Travis Evans
Yo team, crank those calves up like you’re pumping a beat! A daily walk plus some ankle circles is the secret sauce for happy veins. Keep that hydration game strong and ditch the sofa marathons. You’ve got this-let’s keep the blood flowing and the varicose drama at bay.
Jessica Hakizimana
Life is a river, and our veins are the channels that keep us moving forward. When we pause to check our risk, we honor the flow and choose to nurture ourselves. The calculator is a gentle reminder that small choices-like a brisk stroll or a balanced meal-cascade into big health dividends. Embrace each step as a meditation on vitality, and let optimism be the compression that supports your journey. Remember, every beat of the heart is an invitation to keep thriving, not just surviving. So keep shining, stay curious, and let the science guide your confidence.