Potassium Control: Manage Levels Safely with Diet, Medications, and Monitoring
When your body struggles with potassium control, the balance of this essential mineral in your blood that affects heart rhythm, muscle function, and nerve signals. Also known as serum potassium, it’s not just about eating bananas—it’s about understanding how your kidneys, meds, and diet work together to keep levels in a safe range. Too much or too little can send your heart into dangerous rhythms, and many people don’t realize they’re at risk until it’s too late.
Low potassium, or hypokalemia, often shows up after using diuretics like furosemide, vomiting, or heavy sweating. You might feel weak, crampy, or notice your heart skipping beats. On the flip side, high potassium, or hyperkalemia, is common in people with kidney disease, diabetes, or those taking ACE inhibitors or potassium-sparing diuretics. It doesn’t always cause symptoms, but it can suddenly stop your heart. That’s why regular blood tests and knowing your meds matter more than ever. You won’t fix potassium issues by popping supplements without a doctor’s order—many over-the-counter products can push levels into danger zones, especially if your kidneys aren’t filtering well.
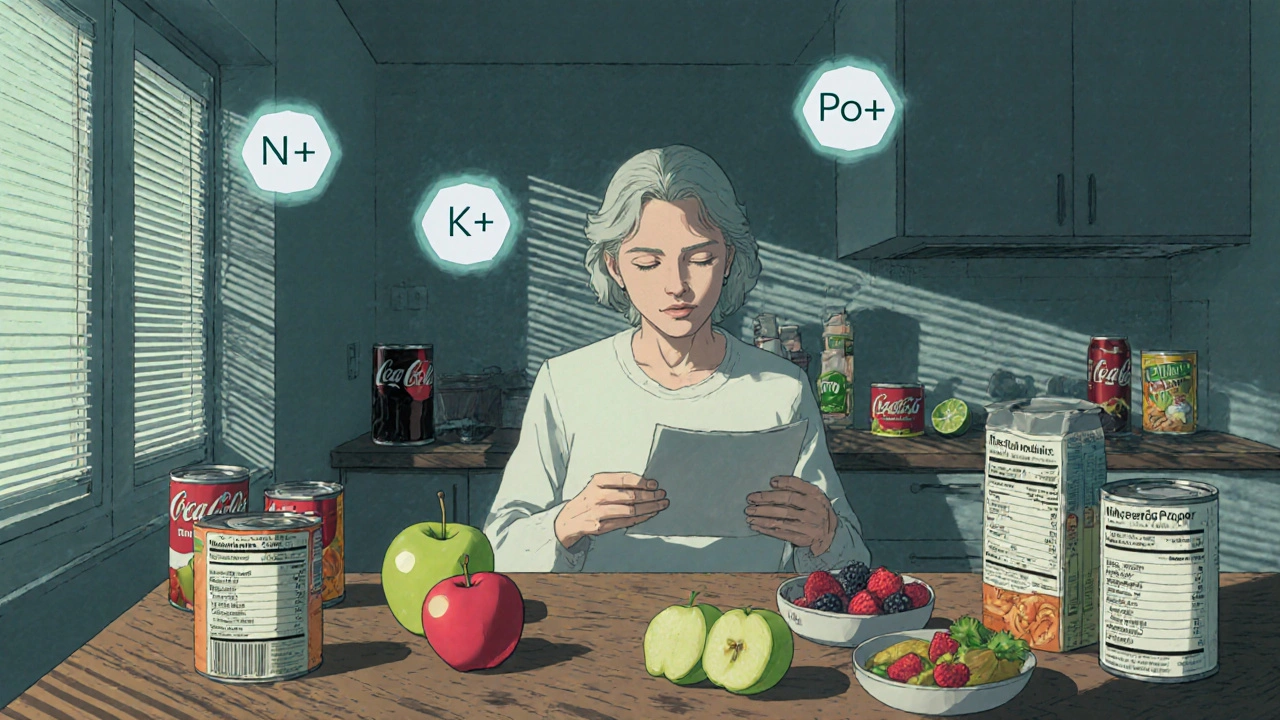
What you eat plays a huge role. Sweet potatoes, spinach, and beans are packed with potassium, but so are salt substitutes and some herbal supplements. If you’re on warfarin, a blood thinner that needs stable vitamin K intake, you’re already tracking food—now add potassium to that list. And if you’re managing heart failure with digoxin, a heart medication that becomes toxic when potassium drops too low, even a small change in your potassium level can make a big difference in how you feel—or if you end up in the ER.
There’s no one-size-fits-all fix. Someone with kidney disease needs to limit potassium, while someone on chronic diuretics might need to boost it carefully. Your doctor will check your levels, adjust your meds, and guide you on what foods to eat—or avoid. It’s not about cutting out all potassium-rich foods, but about consistency and awareness. The posts below cover exactly that: how medications like torsemide, furosemide, and digoxin interact with potassium, how diet changes can help, and what tests you should ask for if you’re at risk. You’ll find real, practical advice—not guesses, not myths, just what works.
Renal Diet Guide: How to Manage Sodium, Potassium, and Phosphorus with Chronic Kidney Disease
Learn how to manage sodium, potassium, and phosphorus with a renal diet for chronic kidney disease. Practical food swaps, expert guidelines, and real-life tips to protect your kidneys and avoid complications.