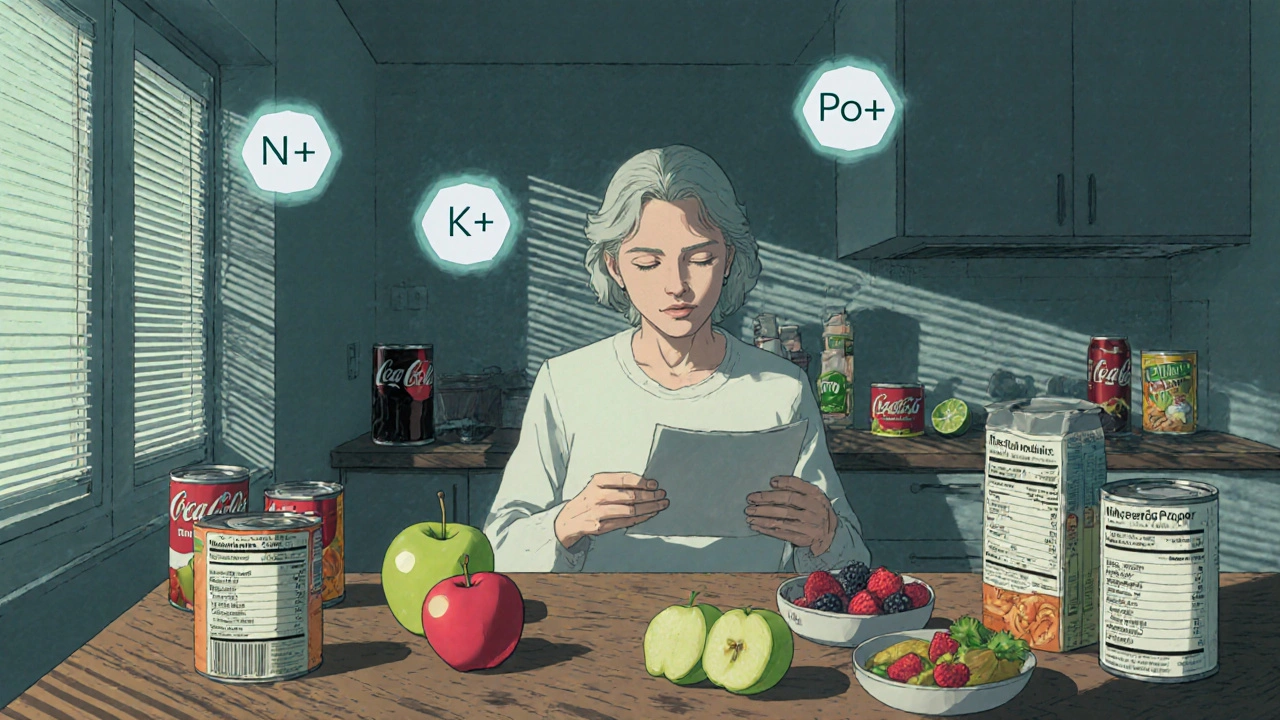
When your kidneys aren’t working well, what you eat becomes just as important as any medication. A renal diet isn’t about losing weight or eating clean-it’s about keeping dangerous minerals from building up in your blood. Too much sodium, potassium, or phosphorus can cause swelling, heart problems, bone damage, and even sudden cardiac arrest. For people with chronic kidney disease (CKD), managing these three minerals isn’t optional. It’s life-saving.
Why Sodium Matters in Kidney Disease
Your kidneys help control fluid balance by filtering out extra sodium. When they’re damaged, sodium sticks around, pulling water with it. That leads to high blood pressure, swollen ankles, shortness of breath, and fluid in the lungs. The goal? Keep sodium under 2,300 milligrams a day-about one teaspoon of salt. But here’s the catch: most sodium doesn’t come from the salt shaker. It comes from packaged and processed foods. A single serving of canned soup can have 800 to 1,200 mg. One slice of processed cheese? Around 400 mg. A fast-food burger? Often over 1,000 mg. Reading labels isn’t just smart-it’s necessary. Swap out salty snacks for fresh fruit, unsalted nuts, or air-popped popcorn. Use herbs like rosemary, thyme, or garlic powder instead of salt. Mrs. Dash and other salt-free blends work well. Cutting sodium by just 1,000 mg a day can lower systolic blood pressure by 5 to 6 mmHg, which reduces strain on your heart and kidneys.Potassium: The Silent Threat
Potassium helps your heart beat regularly. But when kidneys can’t remove it, levels climb dangerously high. A reading above 5.5 mEq/L can trigger irregular heart rhythms-and sometimes, sudden death. That’s why many CKD patients need to limit potassium to 2,000-3,000 mg daily, depending on blood test results. High-potassium foods are often considered healthy: bananas, oranges, potatoes, tomatoes, spinach, beans, and avocados. But they’re risky for people with kidney disease. A medium banana has 422 mg. One cup of cooked spinach? Over 800 mg. The fix? Choose low-potassium options. Apples (150 mg each), berries (65 mg per ½ cup blueberries), cabbage (12 mg per ½ cup cooked), and green beans are safe. Leaching vegetables can cut potassium by half: peel, slice thin, soak in warm water for 2-4 hours, then boil in lots of water and drain. This works for potatoes, carrots, and beets. Also, remember this: potassium from animal foods (meat, dairy) is absorbed more easily than from plants. So even if you eat plant-based foods, portion control still matters. A small serving of salmon or chicken is fine-two to three times a week-but avoid large portions.Phosphorus: The Hidden Problem
Phosphorus helps build bones, but when it builds up in your blood, it pulls calcium out of your bones and deposits it in your blood vessels, heart, and skin. This leads to weak bones, itchy skin, and heart disease. The target? 800-1,000 mg per day for non-dialysis CKD patients. But here’s the twist: not all phosphorus is the same. Natural phosphorus in foods like meat, dairy, and nuts is only 50-70% absorbed. But inorganic phosphorus-added to processed foods-is 90-100% absorbed. That’s why colas, processed cheeses, deli meats, and packaged baked goods are dangerous. A 12-ounce cola has 450 mg. One slice of processed cheese? 250 mg. Even some breads and cereals have added phosphorus under names like “calcium phosphate” or “sodium phosphates.” Choose better options: fresh meats over processed ones, white bread over whole grain (60 mg vs. 150 mg per slice), and plain yogurt instead of flavored. Milk has 125 mg per ½ cup-small amounts are okay. Avoid dairy alternatives like almond or soy milk unless they’re labeled “phosphorus-free.”
Real Food Swaps That Work
Changing your diet doesn’t mean eating bland, boring food. It means making smarter choices. Here are real swaps that people with CKD use daily:- Instead of white potatoes: try cauliflower or green beans
- Instead of orange juice: choose apple or cranberry juice (check labels for added potassium)
- Instead of salted nuts: try unsalted popcorn or rice cakes
- Instead of canned vegetables: use fresh or frozen (rinse canned ones to remove sodium)
- Instead of regular bread: pick white bread or low-phosphorus options
- Instead of soda: drink water, herbal tea, or lemon-infused water
Fluids and Other Considerations
Many people with advanced CKD also need to limit fluids. If you’re making less than 1 liter of urine a day, you may need to cap intake at 32 ounces (about 1 liter). That includes water, coffee, tea, soup, ice cream, and even gelatin. Too much fluid can cause swelling, high blood pressure, and trouble breathing. Protein intake needs balance, too. Too little can lead to muscle loss and malnutrition-especially in older adults. The current recommendation is 0.55 to 0.8 grams of high-quality protein per kilogram of body weight. That means a 70 kg person needs about 40-55 grams daily. Good sources: eggs, lean chicken, fish, and small portions of tofu.What’s New in Renal Nutrition
The field is evolving. In 2023, the FDA approved the first medical food for CKD called Keto-1, which provides essential amino acids without high phosphorus or potassium. Researchers are also testing prebiotic fibers like inulin, which may reduce phosphorus absorption by 15-20%. Digital tools are helping, too. The Kidney Kitchen app, downloaded over 250,000 times, lets you scan barcodes and track nutrients in real time. Mayo Clinic is piloting AI apps that adjust diet suggestions based on your latest lab results-something that could change how we manage CKD long-term. But not all experts agree. Some European guidelines suggest less strict phosphorus limits (up to 1,200 mg/day), arguing that extreme restriction doesn’t improve survival. The key takeaway? Personalization matters. Your diet should be tailored to your lab values, stage of disease, and lifestyle-not a one-size-fits-all plan.
Common Mistakes to Avoid
People often make these errors:- Thinking “natural” means safe-like drinking coconut water (high in potassium) or eating salt substitutes (often contain potassium chloride)
- Skipping meals to cut calories, leading to muscle wasting
- Using bottled salad dressings (loaded with sodium and phosphorus)
- Believing they can eat healthy foods without checking nutrient content-like sweet potatoes or dried fruit
- Not tracking portions-eating “a little” of many high-potassium foods adds up fast
When to See a Renal Dietitian
Medicare now covers 3-6 sessions per year with a registered dietitian for stage 4 CKD patients. A renal dietitian doesn’t just give you a list-they help you adapt. They’ll show you how to read labels, plan meals around your schedule, and adjust based on your blood tests. Most patients take 3-6 months to get comfortable with the diet. It’s hard at first, but it gets easier.Final Thoughts
A renal diet isn’t punishment. It’s control. It’s about keeping your body stable, avoiding hospital visits, and staying off dialysis as long as possible. Studies show proper dietary management can delay dialysis by 6-12 months in stage 4 CKD patients. Start small. Pick one mineral to focus on this week-maybe sodium. Read labels. Swap one high-sodium food for a better choice. Next week, tackle potassium. Slowly, these changes become habits. And habits save lives.Can I still eat fruits and vegetables on a renal diet?
Yes-but you need to choose wisely. Low-potassium options like apples, berries, cabbage, green beans, and cauliflower are safe. Avoid high-potassium ones like bananas, oranges, potatoes, spinach, and tomatoes. Leaching (soaking and boiling) can reduce potassium in some vegetables by up to 50%. Portion control matters-even low-potassium foods can add up if eaten in large amounts.
Is sea salt or kosher salt better than table salt for a renal diet?
No. All types of salt-table, sea, kosher, Himalayan-are made of sodium chloride. They all contain the same amount of sodium per teaspoon. The difference is in texture and flavor, not sodium content. If you’re on a renal diet, you should limit all salt, regardless of type. Use herbs, spices, or salt-free blends instead.
Can I drink milk on a renal diet?
Small amounts are okay, but milk is high in both phosphorus and potassium. One half-cup has 125 mg of phosphorus and 180 mg of potassium. If you need to limit these, choose unsweetened rice milk or almond milk labeled “phosphorus-free.” Avoid dairy alternatives with added phosphates. Always check the ingredient list for “phosphate” or “calcium phosphate.”
Do I need to avoid protein on a renal diet?
No-unless you’re in late-stage CKD and your doctor advises it. Too little protein can cause muscle loss and malnutrition, especially in older adults. The goal is to eat the right amount: 0.55 to 0.8 grams per kilogram of body weight daily. Focus on high-quality sources like eggs, lean chicken, fish, and tofu. Avoid processed meats like bacon or deli meats, which are high in sodium and phosphorus additives.
How do I know if my renal diet is working?
Your blood tests will tell you. Regular checks for sodium, potassium, phosphorus, and creatinine levels show if your diet is effective. Stable or improving numbers mean you’re on track. You’ll also notice less swelling, better blood pressure control, and more energy. If your potassium or phosphorus levels keep rising, your dietitian may need to adjust your plan.
Can I eat out at restaurants on a renal diet?
Yes, but you need to plan ahead. Ask for meals without added salt. Request sauces and dressings on the side. Choose grilled chicken, fish, or lean steak. Avoid fried foods, soups, and anything labeled “seasoned” or “marinated.” Skip sides like mashed potatoes or steamed broccoli (high in potassium). Opt for white rice or pasta instead of whole grains. Many restaurants will accommodate these requests if you ask politely.
Are there any supplements I should avoid?
Yes. Avoid potassium supplements, phosphorus supplements, and multivitamins that contain potassium or phosphorus. Many over-the-counter supplements-even those labeled “natural” or “herbal”-can contain hidden minerals. Always check with your nephrologist or dietitian before taking any supplement. Some renal-specific vitamins are formulated to be safe for CKD patients.
What if I have diabetes too?
It’s challenging. Many heart-healthy foods for diabetics-like fruits, whole grains, beans, and nuts-are high in potassium or phosphorus. Work with a dietitian who specializes in both diabetes and kidney disease. Focus on low-potassium fruits (apples, berries), controlled portions of whole grains, and lean proteins. Blood sugar control is still critical-it’s the leading cause of kidney disease. Balancing both diets takes planning, but it’s doable.
Peter Aultman
Been on this diet for 18 months now and honestly it’s way easier than people make it out to be
Start with swapping soda for lemon water and reading labels on bread
That one change alone cut my sodium by half
No need to overhaul everything at once
gent wood
This is the kind of clear, practical guide that actually helps people
Too many articles just scare you with stats without giving real solutions
Love the leaching tip for potatoes-never knew that worked so well
And yes, processed cheese is the silent killer-every slice is a phosphorus bomb
Thanks for laying it out without the fluff
Barry Sanders
Anyone else notice how every ‘renal diet’ guide ignores that most people can’t afford fresh produce?
And ‘avoid colas’? Sure, when you’re not choosing between insulin and a six-pack of Diet Coke
This is rich people medicine dressed up as health advice
Dilip Patel
lol u think this is hard?? in india we’ve been eating low potassium food for generations
no one eats bananas like americans do
we eat rice dal roti and chutney with zero phosphorus
u think your white bread is better? pfft
our grandmas knew this before u were born
stop overcomplicating things with your fancy apps and labels
just eat real food and stop buying packaged junk
and yes sea salt is still salt u idiot
Nathan Hsu
Let me just say-I’m Indian, and I’ve been doing this for five years-
And I can confirm: the leaching method? Works. I do it with potatoes and carrots every Sunday.
And yes, I still eat bananas-but only half, once a week, and I pair it with a low-potassium meal.
Also, avoid coconut water like the plague-it’s potassium on steroids.
And please, for the love of God, don’t use potassium chloride salt substitutes-they’re worse than table salt.
Also, if you’re on dialysis, you need to track fluid like it’s your job.
One cup of tea? Fine. Two? Maybe. Three? You’re asking for trouble.
And don’t get me started on protein powders-most are loaded with phosphorus.
Stick to eggs, chicken, and tofu.
And if you’re confused, ask your dietitian-they’re not just there to judge you.
It’s not about perfection. It’s about consistency.
And yes, I’ve lost 20 pounds and feel better than I have in a decade.
It’s not a punishment. It’s a lifeline.
Jane Johnson
While the information presented is technically accurate, it fails to account for socioeconomic disparities in access to fresh produce and renal-specific food products.
Furthermore, the emphasis on individual responsibility obscures systemic failures in food policy and healthcare accessibility.
It is therefore ethically questionable to frame dietary adherence as a personal victory without addressing structural inequities.
Sean Hwang
Yeah but you can still eat good food
I make stir fry with cabbage, chicken, and rice
Use soy sauce sparingly and add ginger and garlic
It tastes amazing and I don’t feel like I’m starving
And yeah I use the Kidney Kitchen app-it’s free and saves so much time
Just pick one thing to change each week
That’s all you need
kshitij pandey
Hey everyone, I’m a CKD patient from India and I’ve been sharing tips in local WhatsApp groups
One thing I tell everyone: don’t panic
Start with cutting out packaged snacks
Swap chips for roasted chana or puffed rice
Use lemon juice and black salt instead of regular salt
And if you can’t find phosphorus-free milk, dilute regular milk with water
Small changes, big results
And you’re not alone-we’ve got each other
Keep going
Brittany C
While the article references FDA-approved medical foods and prebiotic fibers, it lacks critical context regarding the evidence hierarchy supporting these interventions.
Keto-1 is a phase II trial product with limited real-world data.
Furthermore, the claim that inulin reduces phosphorus absorption by 15–20% is derived from murine models and has not been replicated in human CKD cohorts.
It is premature to recommend these as standard interventions without larger RCTs.
Chris Ashley
Just had my first meal on this diet and I’m already hungry
Why can’t I just eat a burger?
It’s not like I’m gonna die tomorrow