Hypertensive Crisis: What It Is, Why It’s Dangerous, and How to Stay Safe
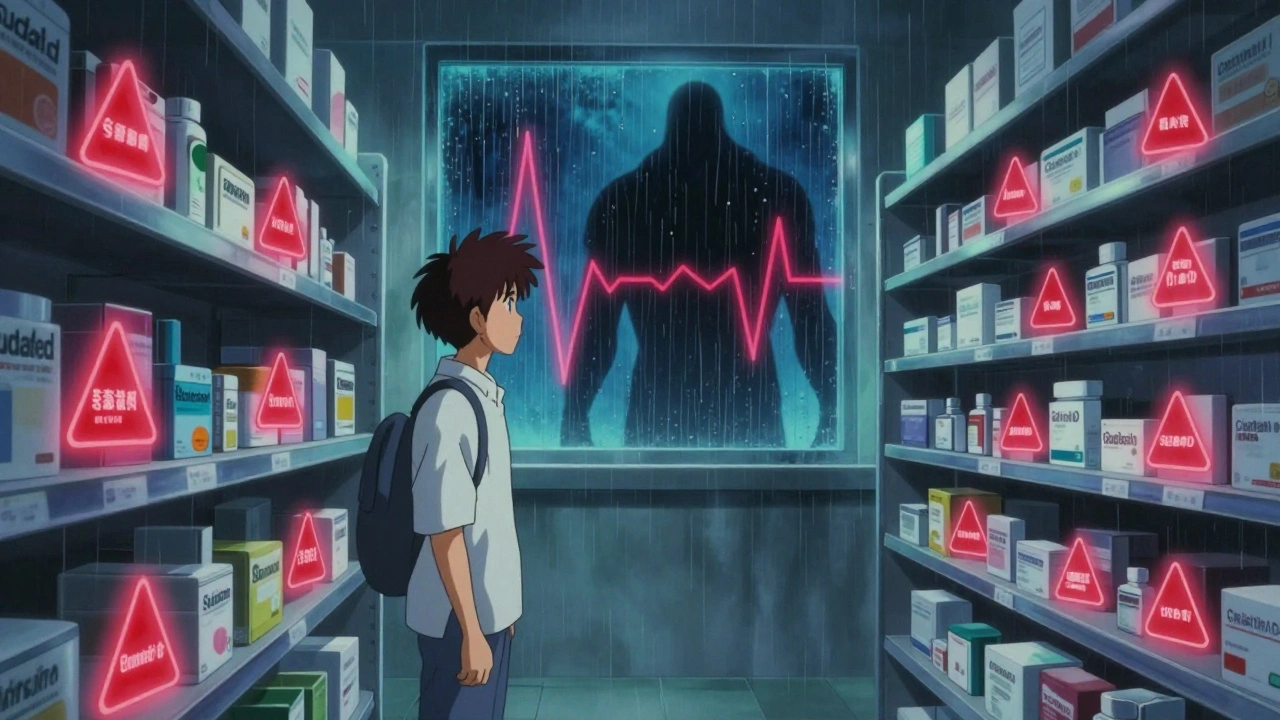
When your blood pressure spikes to dangerous levels—usually above 180/120 mm Hg—you’re facing a hypertensive crisis, a sudden, severe rise in blood pressure that can damage organs and lead to stroke, heart attack, or kidney failure. Also known as hypertensive emergency, this isn’t just a bad day with high numbers—it’s a medical emergency that needs treatment within minutes to hours. Unlike routine high blood pressure, which builds slowly over years, a hypertensive crisis happens fast and often without clear warning signs. Many people don’t feel anything until their body starts shutting down.
This isn’t just about numbers. A hypertensive crisis, a sudden, severe rise in blood pressure that can damage organs and lead to stroke, heart attack, or kidney failure. Also known as hypertensive emergency, this isn’t just a bad day with high numbers—it’s a medical emergency that needs treatment within minutes to hours. Many people don’t feel anything until their body starts shutting down.
What causes it? Often, it’s someone skipping their blood pressure meds, using stimulants like cocaine or amphetamines, or having uncontrolled secondary hypertension from kidney disease or adrenal tumors. Some cases happen after stopping beta-blockers too quickly. It can also be triggered by preeclampsia during pregnancy or severe pain. The key is recognizing that blood pressure medications, drugs like labetalol, nitroprusside, or nifedipine used to rapidly lower dangerously high readings in emergency settings aren’t just for daily control—they’re life-saving tools in a crisis.
Not every high reading means crisis. If your pressure is sky-high but you feel fine and have no signs of organ damage—like chest pain, confusion, vision changes, or shortness of breath—it’s called a hypertensive urgency, a severe elevation in blood pressure without acute organ damage, requiring prompt but not immediate treatment. This still needs attention within 24 to 48 hours, but it’s not an ambulance situation. The difference between urgency and emergency can be the difference between a doctor’s visit and an ICU stay.
People on blood pressure meds should never stop them cold. If you miss a dose, don’t double up. If you feel dizzy, lightheaded, or notice your usual symptoms returning, check your pressure and call your provider. Keep a home monitor. Know your numbers. And if you ever feel like your head might explode, your chest is crushing, or you can’t see clearly—don’t wait. Call 911. That’s not panic. That’s survival.
The posts below cover real-world scenarios you might not expect: how certain drugs like antidepressants or decongestants can push someone into crisis, why kidney disease makes high blood pressure more dangerous, and how to use interaction checkers to avoid deadly combos. You’ll find practical guides on managing meds safely, spotting early signs, and what to do if you’re caring for someone at risk. This isn’t theory—it’s what works when every minute counts.
MAOIs and OTC Cold Medicines: What You Need to Know About Hypertensive Crisis and Serotonin Risks
MAOIs for depression can cause life-threatening reactions when mixed with common OTC cold medicines. Learn which ingredients to avoid, what symptoms to watch for, and safe alternatives to stay healthy without risking hypertensive crisis or serotonin syndrome.