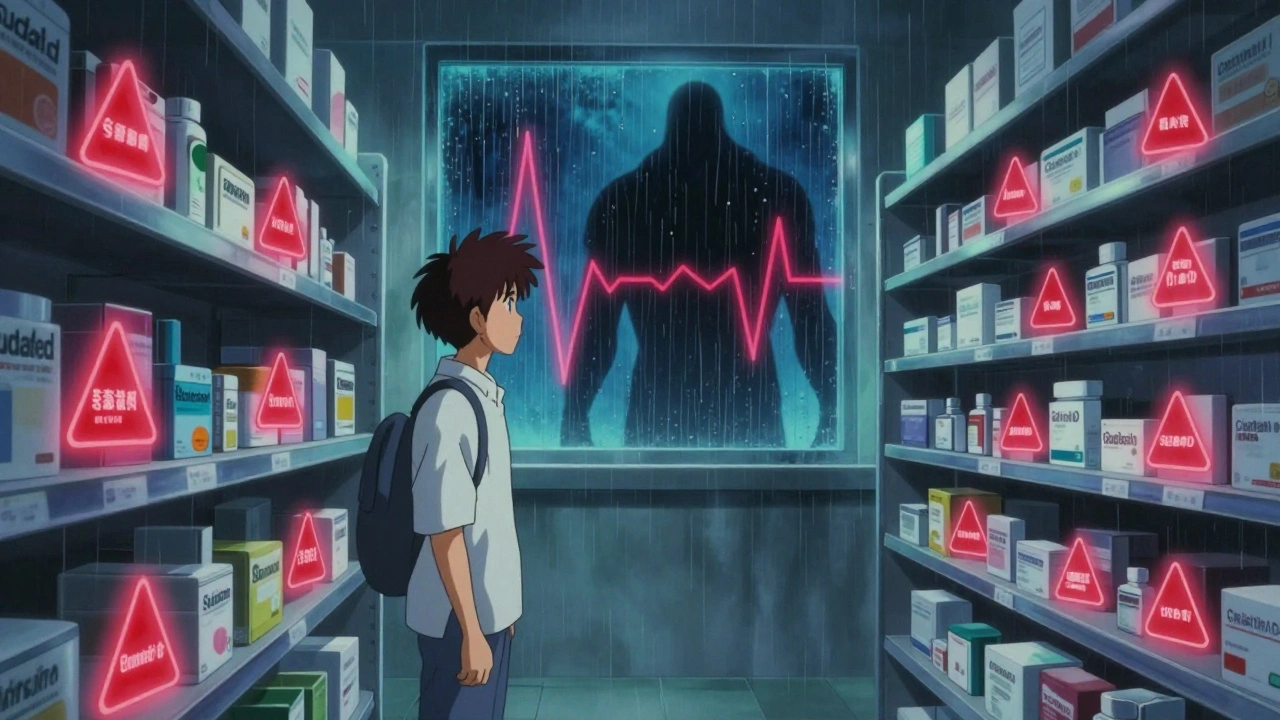
MAOI Cold Medicine Safety Checker
Check Cold Medicine Safety
Enter the name of a cold medicine or active ingredient to see if it's safe with MAOIs. Never take OTC cold meds without checking.
If you're taking an MAOI for depression, a simple cold medicine could send you to the emergency room. This isn't a hypothetical risk-it's a real, documented danger that has landed people in intensive care after taking something as common as Sudafed or Robitussin DM. The combination of monoamine oxidase inhibitors (MAOIs) and over-the-counter cold medications can trigger a hypertensive crisis or serotonin syndrome, two life-threatening conditions that develop fast and demand immediate medical attention.
Why MAOIs Are Different
MAOIs like phenelzine (Nardil), tranylcypromine (Parnate), and isocarboxazid (Marplan) work by blocking the enzyme that breaks down neurotransmitters like serotonin, norepinephrine, and dopamine. This helps lift depression, especially in cases where other antidepressants have failed. But that same mechanism makes them dangerously sensitive to certain chemicals found in everyday cold and flu products. Unlike SSRIs or SNRIs, which mostly affect serotonin reuptake, MAOIs permanently disable the body’s ability to clear out excess neurotransmitters and stimulants. That means when you take a decongestant like pseudoephedrine or phenylephrine, your body can’t process the surge of norepinephrine it releases. The result? Blood pressure spikes uncontrollably. Even the transdermal selegiline patch (Emsam), which has fewer dietary restrictions at low doses, still carries the same interaction risks with OTC cold medicines. There’s no safe version of an MAOI when it comes to these drugs.The Dangerous Ingredients in OTC Cold Medicines
You won’t find a warning label on the box that says "Do not use if you take MAOIs." That’s the problem. These ingredients are hidden in multi-symptom formulas under confusing names. Here’s what to avoid:- Pseudoephedrine - Found in Sudafed, Zyrtec-D, Claritin-D
- Phenylephrine - Found in Sudafed PE, Robitussin Peak Cold, many "new" decongestants
- Dextromethorphan - Found in Robitussin DM, Delsym, NyQuil, DayQuil
- Phenylpropanolamine - Banned in the U.S. since 2000, but still found in some imported or older products
Hypertensive Crisis: The Silent Emergency
A hypertensive crisis happens when your blood pressure spikes above 180/120 mmHg. With MAOIs and decongestants, it can hit 220/110 or higher within hours. Symptoms include:- Severe headache, often at the back of the head
- Blurred vision or seeing spots
- Chest pain or tightness
- Palpitations or racing heartbeat
- Nausea, vomiting, or sweating
- Stiff neck or confusion
Serotonin Syndrome: When Your Brain Overloads
Dextromethorphan, a common cough suppressant, is a serotonergic agent. When combined with an MAOI, it pushes serotonin levels far beyond what your brain can handle. This isn’t just a bad reaction-it’s a neurological emergency. Symptoms of serotonin syndrome include:- Agitation, restlessness, or confusion
- Fast heart rate, high blood pressure
- High body temperature (over 101°F)
- Muscle rigidity, twitching, or tremors
- Loss of coordination, stumbling
- Diarrhea, sweating, shivering

What You Can Safely Take Instead
You don’t have to suffer through a cold untreated. Safe alternatives exist:- For cough: Guaifenesin (Mucinex) - breaks up mucus, no interaction risk
- For fever or pain: Acetaminophen (Tylenol) - safe at standard doses
- For runny nose: Saline nasal spray - no drugs, just salt water
- For congestion: Steam inhalation or humidifier - natural, effective, zero risk
How to Stay Safe: A Practical Checklist
If you’re on an MAOI, follow these steps every time you reach for an OTC medicine:- Read the "Active Ingredients" label-not the brand name or marketing claims.
- Look for pseudoephedrine, phenylephrine, or dextromethorphan.
- If you see any of those, put it back.
- Ask your pharmacist: "Is this safe with MAOIs?" Don’t assume they know-many aren’t trained on this specific risk.
- Keep a printed list of unsafe drugs in your wallet. Many patients report this saved them after forgetting details.
- When in doubt, wait it out. A cold lasts a week. A hypertensive crisis can kill you in minutes.
Why This Risk Is Still So Common
MAOIs make up less than 1% of all antidepressant prescriptions in the U.S. But for the people who need them, they’re often the only option that works. A 2023 Mayo Clinic study found that in treatment-resistant depression, MAOIs have over a 50% response rate-much higher than SSRIs. The problem? Most doctors assume patients know the risks. They don’t. A 2021 University of North Carolina study showed patients need 3 to 5 separate educational sessions just to understand the dangers. Many are never warned properly. Even worse, OTC drug labels don’t mention MAOIs. The FDA requires black box warnings on MAOI packaging, but those are ignored by consumers. And because MAOIs are rarely prescribed, pharmacists may not think to ask.
What’s Changing
New research is pushing for better safety protocols. A June 2023 study in JAMA Psychiatry showed that even a single 30mg dose of pseudoephedrine caused an average blood pressure spike of 42/28 mmHg in patients on phenelzine. That’s enough to trigger a crisis in vulnerable people. There’s also hope on the horizon. A new reversible MAO-A inhibitor called CX-1010 is in Phase II trials (NCT04567812). If successful, it could offer the same benefits as MAOIs without the deadly interactions. But until then, the rules haven’t changed. The same warnings from the FDA’s 1976 expert panel still stand: "Patients taking MAOIs should not take nasal decongestants orally except under the advice and supervision of a physician."Real Stories, Real Consequences
One user on PatientsLikeMe shared how their psychiatrist gave them a wallet-sized card listing every unsafe OTC drug. "I’ve used it five times to avoid buying the wrong medicine," they wrote. "It’s saved me from ER visits." Another user on Psych Forums described 12 hours of severe headache, neck stiffness, and heart palpitations after taking DayQuil with Nardil. "I thought I was dying. I called 911. They said I had a hypertensive episode. I didn’t even know DayQuil had pseudoephedrine." These aren’t rare outliers. They’re preventable tragedies.Final Word
MAOIs are powerful tools for depression that don’t respond to other treatments. But they come with non-negotiable safety rules. Ignoring them isn’t an accident-it’s a gamble with your life. There’s no "maybe" here. If you’re on an MAOI, you cannot take any OTC cold medicine without checking every single active ingredient. No exceptions. No "just this once." Your health isn’t worth the risk. And there are safe ways to manage a cold without putting yourself in danger.Can I take Tylenol with MAOIs?
Yes, acetaminophen (Tylenol) is safe to use with MAOIs for pain or fever. It doesn’t affect neurotransmitter levels or blood pressure in a way that interacts with MAOIs. Stick to the recommended dose-no more than 3,000 mg per day-and avoid combination products that include decongestants or cough suppressants.
Is Sudafed PE safe with MAOIs?
No, Sudafed PE contains phenylephrine, which is just as dangerous as pseudoephedrine when taken with MAOIs. Even though it replaced pseudoephedrine in many products, phenylephrine still triggers a dangerous rise in blood pressure in people on MAOIs. Avoid all forms of phenylephrine.
What about Zyrtec-D or Claritin-D?
No. Both Zyrtec-D and Claritin-D contain pseudoephedrine or phenylephrine. Even if you only take them for allergies, they’re unsafe with MAOIs. Use plain Zyrtec or Claritin (without the "D") instead. Always check the active ingredients, not the brand name.
Can I use nasal sprays instead of oral decongestants?
Some nasal sprays are safer, but not all. Oxymetazoline (Afrin) and phenylephrine nasal sprays can still be absorbed into your bloodstream and cause problems. The safest option is saline nasal spray-no drugs, no risk. If you must use a medicated spray, talk to your doctor first and limit use to 3 days max.
How long do I have to wait after stopping an MAOI before taking OTC cold medicine?
Wait at least 14 days after stopping any MAOI before taking any decongestant or dextromethorphan-containing product. This is because most MAOIs irreversibly block the enzyme, and it takes weeks for your body to make new enzymes. The American Psychiatric Association recommends this 14-day washout period to prevent serotonin syndrome or hypertensive crisis.
Are there any OTC cold medicines that are definitely safe?
Yes, but you must read labels carefully. Safe options include: guaifenesin (Mucinex) for chest congestion, acetaminophen (Tylenol) for pain/fever, and saline nasal spray for congestion. Avoid anything with "DM," "D," "Multi-Symptom," or "Nighttime." If the label lists more than one active ingredient, skip it.
What should I do if I accidentally took a dangerous OTC medicine?
Call 911 or go to the nearest emergency room immediately. Do not wait for symptoms to appear. Hypertensive crisis and serotonin syndrome can develop within hours. Tell the medical team you’re on an MAOI and what you took. Bring the medicine bottle with you. Early treatment can save your life.
Can my pharmacist help me pick safe OTC medicines?
Yes-but don’t assume they will. Many pharmacists aren’t trained on MAOI interactions. Bring your own list of unsafe ingredients and ask: "Is this safe with MAOIs?" If they’re unsure, ask them to check a reliable drug interaction database. Some pharmacies offer free medication reviews for patients on complex regimens-ask about it.
Is it safe to take herbal cold remedies like echinacea or zinc with MAOIs?
There’s not enough data to say they’re safe. Some herbal products can affect serotonin or blood pressure, and they’re not regulated like drugs. Stick to proven, single-ingredient, non-pharmacological options like rest, hydration, saline spray, and humidifiers. If you want to try an herbal remedy, talk to your doctor first.
Why aren’t these warnings on OTC medicine labels?
OTC labels are designed for the general public, not people on rare psychiatric medications. The FDA requires MAOI packaging to have black box warnings, but not the reverse. This gap leaves patients vulnerable. That’s why patient education and personal vigilance are critical. Always check active ingredients yourself-don’t rely on labels alone.
Marvin Gordon
This is the kind of post that saves lives. I’m on Parnate and I used to grab Sudafed like it was candy. Now I keep a printed list in my wallet. No more guessing. Seriously, if you’re on an MAOI, treat every OTC med like a landmine. It’s not hype-it’s survival.
ashlie perry
They dont want you to know this but the FDA and pharma are hiding this because they make more money off ER visits and hospital stays. They let you die quietly so you dont sue them. Wake up.
Norene Fulwiler
I’m from Mexico and we don’t have the same OTC rules here. I’ve seen people in my family take NyQuil with antidepressants and just shrug it off. This post is a wake-up call for so many cultures that don’t treat meds like science. Thank you for writing this.
Ada Maklagina
I took DayQuil with Nardil once. Thought I was just having a bad anxiety day. Turns out my BP was 210/105. ER nurse said if I’d waited another hour I might’ve had a stroke. I don’t touch anything with a D anymore. Ever.
Stephanie Fiero
I cant believe people still dont get this. Its not rocket science. Read the label. If it says D or DM its poison. I had to explain this to my mom 3 times. She thought "natural" meant safe. Natural can kill you too. I print this out and tape it to my fridge.
Laura Saye
There’s a deeper layer here. The isolation of being on an MAOI isn’t just medical-it’s existential. You’re told you’re lucky to have a tool that works, but then you’re forced to live like a hermit, avoiding everything from cough syrup to birthday cake with hidden sugars. The system doesn’t design for the rare. It designs for the majority. And the majority doesn’t care until it’s their kid in the ICU.
sean whitfield
Oh wow another PSA from the medical industrial complex. Next they’ll tell me not to breathe near a decongestant. Wake up sheeple. The real danger is trusting a pill to fix your brain. Maybe just go outside and yell into a pillow instead.
Stephanie Bodde
I’m so proud of you for sharing this 💪 I know how scary it is to be the only one who gets it. You’re not alone. I’ve been on Nardil for 8 years and I carry a laminated card too. We got this 🙌
Jennifer Patrician
This is all fearmongering. I’ve been on MAOIs for 15 years and I take Robitussin DM every winter. Nothing happened. The real problem is doctors scaring people into compliance. You’re not a lab rat. Take your medicine and live your life.
Ali Bradshaw
I’m in the UK and we have way fewer OTC decongestants on shelves here. It’s actually easier. I’ve never had to worry about this. Maybe the US needs better regulation. Not just patient education.
Lynette Myles
Pseudoephedrine and phenylephrine are both alpha-1 agonists. They directly stimulate vascular smooth muscle. MAOIs prevent norepinephrine reuptake and degradation. Synergistic vasoconstriction. BP spikes are inevitable. No exceptions.
Jimmy Jude
I’ve seen people die from this. Not because they were careless. Because their doctor didn’t warn them. I’m a psychiatrist. I’ve had patients show up in cardiac arrest because they took NyQuil thinking it was "just a cold." You don’t get a second chance. This isn’t advice. It’s a last will and testament.