DVT Risk Factors
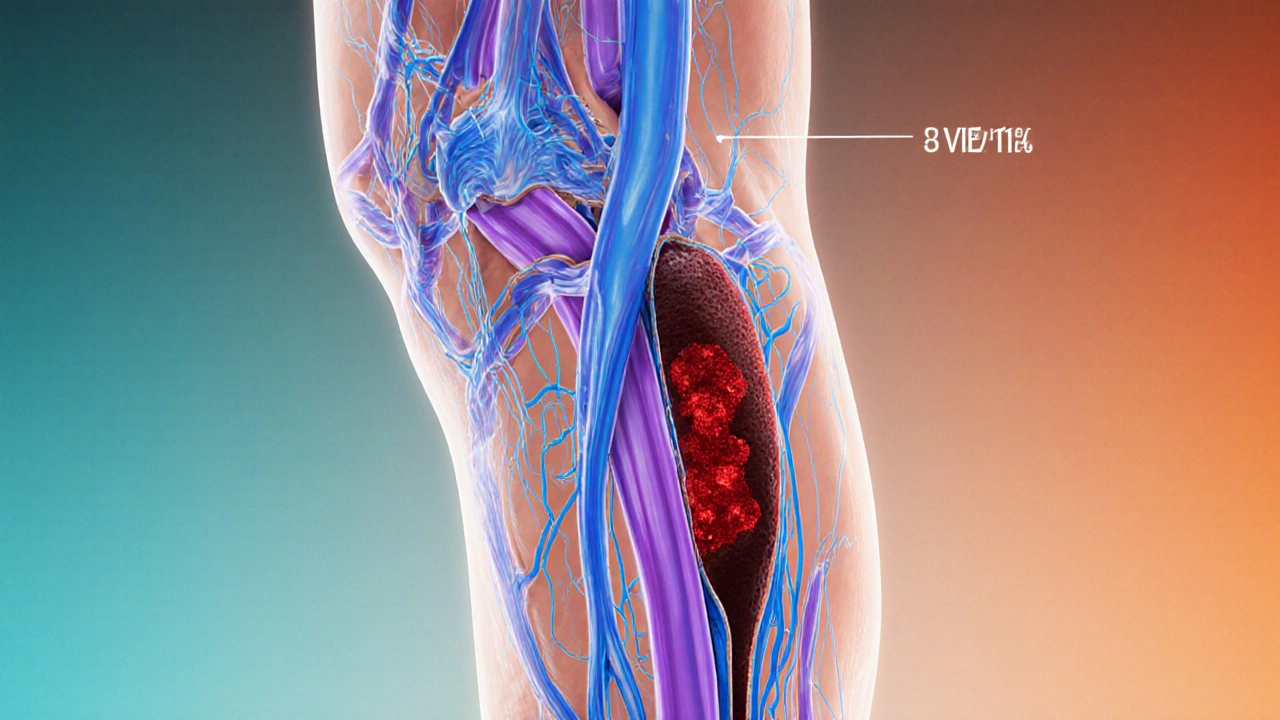
When talking about DVT risk factors, the main causes that raise the chance of developing a deep vein clot. Also called deep vein thrombosis causes, they shape who gets a clot and why. A related condition is Deep Vein Thrombosis (DVT), a blood clot that forms in the deep veins, most often in the legs. Understanding the risk factors helps you spot trouble early and act before a clot becomes dangerous.
Key Elements of DVT Risk
The classic trio that doctors use to explain clot formation is called Virchow’s triad. It says that DVT risk factors encompass three ideas: Venous Stasis, slow or pooled blood flow in the legs, Hypercoagulability, a blood‑clot‑prone state caused by genetics or medication, and damage to the vein lining, known as endothelial injury. In plain words, if blood isn’t moving, if it’s extra sticky, or if the vein wall is hurt, the risk of a clot jumps.
First, think about everyday moments that cause venous stasis. Long flights, marathon road trips, or even a day at the desk without standing up can let blood pool in the calves. That pooling is why you might feel a sore or a heavy feeling after a long journey. Simple moves—like stretching every hour or taking a quick walk—keep the blood flowing and cut the stasis effect.
Second, hypercoagulability often hides behind medical labels. Conditions such as cancer, inflammatory bowel disease, or certain autoimmune disorders make the blood extra clutchy. Hormonal factors play a big part too: birth‑control pills, hormone replacement therapy, and pregnancy all boost clot‑forming proteins. Even a family history of clotting disorders—like Factor V Leiden or protein C deficiency—means your blood may be wired to clot more easily.
Third, injury to the vein lining can happen from surgery, especially hip or knee replacements, or from a fracture that damages deep veins. Even a minor cut that inflames a vein can tip the balance toward clotting. In these cases, doctors often prescribe blood thinners right after the procedure to prevent the clot from forming.
Beyond the core triad, lifestyle habits add extra layers. Being overweight squeezes the veins, making flow harder. Smoking damages the endothelial cells, turning them into a sticky landing pad for clots. A diet low in fiber and rich in processed foods can increase inflammation, indirectly nudging clot risk upward. Each habit is a small push, but together they can create a significant problem.
What can you do to lower the odds? Start with movement: set a timer to stand, stretch, or walk for a few minutes every hour if you sit a lot. Stay hydrated—water keeps the blood thinner. If you’re traveling, wear graduated compression socks; they gently squeeze the leg and encourage blood back toward the heart. For people with known clotting disorders or recent surgery, follow your doctor’s plan for anticoagulants or blood thinners without skipping doses.
Know the warning signs, too. Sudden swelling, warmth, redness, or pain in one leg should raise an alarm. If you feel any of these, especially after a period of inactivity or surgery, seek medical help right away. Early diagnosis and treatment can stop a clot from traveling to the lungs, which can be life‑threatening.
All these points set the stage for the articles you’ll see below. They dive deeper into specific risk categories—like how hormone therapy influences clotting, or what genetic tests can reveal—plus practical guides on buying affordable meds that can help manage or prevent DVT. Keep reading to get targeted advice, real‑world tips, and the latest updates on staying clot‑free.
Deep Vein Thrombosis and Varicose Veins: How They're Linked and What to Do
Explore how varicose veins and deep vein thrombosis are connected, learn shared risk factors, symptoms to watch for, and practical steps to prevent serious complications.