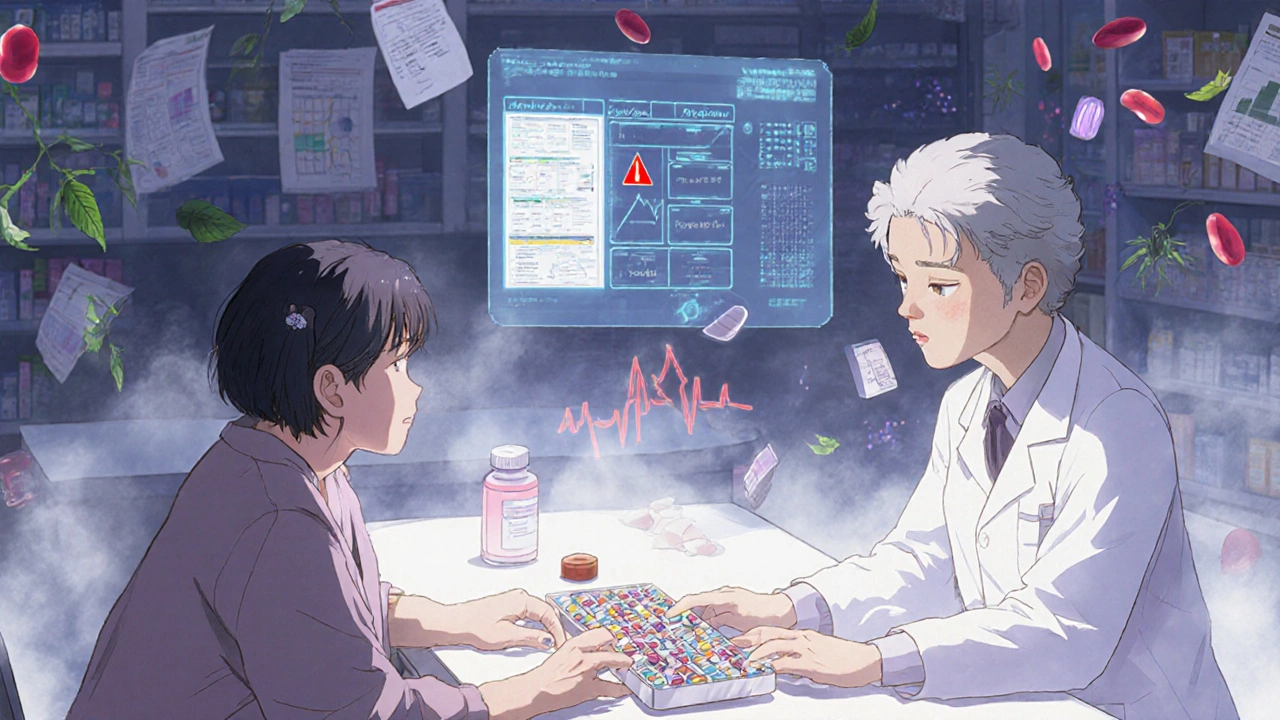
Every year, over 1.5 million avoidable adverse drug events happen in U.S. hospitals alone. Many of these are caused by simple, unnoticed interactions between medications you’re already taking. A drug interaction checker isn’t just a fancy tool-it’s a safety net. Whether you’re on five prescriptions, take supplements, or mix over-the-counter painkillers with your blood thinner, knowing how to use one correctly can prevent hospital visits, bleeding, kidney damage, or worse.
What Is a Drug Interaction Checker?
A drug interaction checker is a digital tool that scans the medications, supplements, or even foods you’re using and flags combinations that could be dangerous. It doesn’t guess-it uses real pharmacology data. For example, mixing warfarin (a blood thinner) with ibuprofen can increase your risk of internal bleeding. A good checker will catch that and tell you why.
These tools come in different forms: some are built into hospital systems like Epic or Cerner, others live in apps like Medisafe, or are web-based like the University of Liverpool’s checker. Some are designed for doctors and pharmacists; others are made for everyday users. The core function is the same: input your drugs, get back a risk report.
Why You Need One (Even If You’re Not a Doctor)
Most people don’t realize how common polypharmacy is. Nearly half of all Americans take at least one prescription drug. Among adults over 65, 44% take five or more medications. That’s a lot of chances for something to go wrong.
Let’s say you take lisinopril for blood pressure, metformin for diabetes, and a daily fish oil supplement. Sounds harmless, right? But fish oil can thin your blood. If you also start taking aspirin for heart health, you’re stacking two blood-thinning agents. No one told you. A drug interaction checker would flag that combo as “moderate risk”-giving you time to talk to your pharmacist before it becomes a problem.
Studies show that when people use these tools, they catch dangerous interactions they’d otherwise miss. One user on Medisafe’s app reported catching a warfarin-ibuprofen combo before it caused a bleed. That’s not luck-that’s using the tool right.
Step 1: Gather Your Full Medication List
Before you open any checker, write down everything you take. Not just prescriptions. Include:
- All prescription drugs (including doses and frequency)
- Over-the-counter meds (ibuprofen, antacids, sleep aids)
- Vitamins and supplements (vitamin D, magnesium, melatonin)
- Herbal products (st. john’s wort, echinacea, ginkgo)
- Recreational substances (alcohol, cannabis-if relevant)
Don’t skip the supplements. St. John’s wort can make birth control, antidepressants, and even some heart meds stop working. Ginkgo can increase bleeding risk with blood thinners. These aren’t “natural” loopholes-they’re active chemicals with real effects.
Pro tip: Use your pharmacy’s printed list. Most pharmacies now print a full medication summary on your pick-up receipt. That’s your starting point.
Step 2: Choose the Right Tool for You
Not all checkers are made equal. Here’s what works best for different users:
- For everyday users: Medisafe (iOS/Android) is simple, free, and lets you save your “Med Cabinet.” It’s designed for people who aren’t medical pros.
- For people on complex regimens: Lexi-Interact or Micromedex (often accessed through your doctor’s portal) are used in hospitals and offer the most detailed data. They’re harder to use alone but more accurate.
- For checking supplements: DrugBank’s API or the University of Liverpool’s tool include supplement interactions, which many consumer apps miss.
- For quick checks: Epocrates (free app) is fast and widely used by clinicians. It’s reliable for common drug pairs.
Don’t rely on Google or random websites. Many online “interaction checkers” are outdated or inaccurate. Stick to tools backed by clinical databases like Micromedex, Lexicomp, or DrugBank.
Step 3: Enter Your Medications Correctly
Here’s where most people mess up. You can’t just type “aspirin.” You need to be specific.
For example:
- “Aspirin” → could mean 81 mg daily or 325 mg for pain
- “Metformin” → is it immediate-release or extended-release?
- “Fish oil” → is it 1,000 mg or 3,000 mg?
Most tools have dropdown menus. Click through them. If the tool doesn’t recognize “ibuprofen 200 mg,” try “Advil” or “Motrin.” Generic names often work better than brand names.
Some systems, like DrugBank, require you to use a unique ID (Product Concept ID) for accuracy. That’s for professionals. For most users, just pick the closest match from the list.
Important: Always include the route-oral, topical, injection. A topical steroid and an oral steroid are different interactions.
Step 4: Read the Results-Don’t Just Panic
Once you hit “check,” you’ll get a color-coded or severity-based result. Here’s what the codes mean:
- Red (Contraindicated): Don’t take these together. Risk of serious harm. Example: statins + grapefruit juice.
- Orange (Significant): Use with caution. May need dose change or monitoring. Example: warfarin + amiodarone.
- Yellow (Mild): Minor effect. Usually no action needed. Example: omeprazole + certain antibiotics.
- Green (No Interaction): Safe together.
Don’t ignore the details. Click every “i” icon or “Learn More” link. It explains why the interaction happens. For example, “This combo increases risk of serotonin syndrome” tells you what to watch for-confusion, rapid heart rate, tremors.
Some tools, like the University of Liverpool’s, use shapes: red circles, orange squares, yellow triangles. Same idea. Learn the system.
Step 5: Don’t Trust It Blindly
Even the best tools miss things. Studies show DDI checkers catch 60-85% of dangerous interactions. That means up to 4 in 10 risky combos fly under the radar.
Why? Because:
- They don’t always know your full health history (kidney disease? liver issues?)
- They can’t account for timing (e.g., taking meds 2 hours apart vs. together)
- They don’t know if you’re drinking alcohol or smoking
- They get confused by similar drug names (e.g., metoprolol vs. metformin)
That’s why experts say: use the checker as a starting point, not the final word. Always talk to your pharmacist or doctor about any flagged interaction-even if it’s just “yellow.”
One study found that 49% of hospital alerts were ignored by clinicians because they were too noisy. That’s alert fatigue. Don’t be that person. If something looks off, ask.
Step 6: Take Action-Don’t Just See It
Seeing a red flag means nothing if you do nothing.
Here’s what to do based on the result:
- Red: Stop the combo immediately. Call your doctor or pharmacist. Don’t wait.
- Orange: Schedule a call with your pharmacist. Ask: “Can I switch one of these? Should I get blood tests?”
- Yellow: Note it in your health journal. Watch for symptoms. Re-check in 2 weeks if you’re still taking both.
- Green: Still good to confirm with your provider if you’re on high-risk meds.
Example: You check your meds and see a red flag between simvastatin and clarithromycin. That combo can cause muscle damage. Your doctor might switch you to pravastatin, which doesn’t interact. That’s the power of this tool.
Common Mistakes People Make
Even with the best tools, users keep making the same errors:
- Only checking one drug at a time. Interactions happen between three or more. Always check your full list together.
- Using outdated apps. If your app hasn’t updated since 2020, it’s missing new data. Check for updates.
- Assuming “natural” means safe. Supplements aren’t regulated like drugs. St. John’s wort interacts with over 50 medications.
- Not updating after a prescription change. If your doctor adds a new med, re-check immediately.
- Ignoring the fine print. “Take with food” or “avoid grapefruit” matters. These are part of the interaction.
One user on Reddit complained about Micromedex giving 30+ false alerts for routine meds. That’s not the tool’s fault-it’s that they didn’t enter their meds correctly. Double-check every entry.
What to Do If the Checker Says Nothing
Just because a checker doesn’t flag something doesn’t mean it’s safe.
For example, many tools still don’t fully track interactions between antidepressants and CBD, or between antibiotics and birth control. Some newer drugs (like semaglutide) have limited interaction data because they’re too new.
If you’re unsure, ask your pharmacist directly. Pharmacists are trained to spot hidden risks. Most will do a free interaction check for you-even if you didn’t buy the meds there.
Keep It Updated
Medication lists change. So should your checker.
- Update your list every time your prescription changes.
- Re-check every 3 months, even if nothing changed.
- Set a calendar reminder: “Med Check” on the first of every quarter.
People who update their lists regularly are 60% less likely to have an adverse event, according to a 2023 study in the Journal of Patient Safety.
Think of it like checking your car’s oil. You don’t wait until it breaks down.
Final Thought: This Is Your Safety Net
Drug interaction checkers aren’t magic. But they’re one of the most effective, low-cost tools you have to protect yourself. You don’t need to be a doctor. You just need to be careful.
Use the right tool. Enter your meds accurately. Read the warnings. Talk to your pharmacist. Update regularly.
That’s it. No complicated steps. No jargon. Just a few habits that can keep you out of the ER.
Can I trust free drug interaction checkers?
Yes, but only if they’re built on trusted databases like Micromedex, Lexicomp, or DrugBank. Apps like Medisafe and Epocrates use these sources and are reliable for personal use. Avoid random websites or apps without clear sources. Free doesn’t mean unsafe-but unverified does.
Do drug interaction checkers work for supplements?
Some do, some don’t. Consumer apps like Medisafe and Epocrates often miss supplements. For better coverage, use DrugBank’s free web tool or the University of Liverpool’s checker. Always assume supplements can interact-especially herbal ones like St. John’s wort, ginkgo, or garlic extract.
What if my doctor says the interaction isn’t a problem?
Ask them why. Doctors sometimes override alerts based on experience-but they should explain the reasoning. If they say “it’s fine,” ask: “What signs should I watch for?” and “Is there a safer alternative?” Don’t accept vague answers. Your safety is your responsibility too.
Can I use a drug interaction checker for my elderly parent?
Absolutely. Seniors are at highest risk for dangerous interactions because they often take 5-10 medications. Use Medisafe or another app with a simple interface. You can create a profile for them and add their meds. Share the results with their pharmacist. It’s one of the best ways to prevent hospitalizations.
How often do these tools get updated?
Reputable tools update their databases monthly or quarterly. Micromedex and Lexicomp add new interaction data as soon as it’s published in medical journals. Consumer apps like Medisafe sync automatically. Always check your app’s update log or settings to confirm it’s current. Outdated tools are worse than no tools.
Do I need to pay for a good drug interaction checker?
No. The best consumer tools-Medisafe, Epocrates, and DrugBank’s web interface-are free. Hospitals pay thousands for advanced systems like Micromedex, but you don’t need those unless you’re a clinician. Stick with free, trusted apps. Paying doesn’t mean better.
Next Steps
Start today. Grab your medication list. Open Medisafe or Epocrates. Add your drugs. Hit check. Read the results. Then call your pharmacist and say, “I ran my meds through a checker-here’s what came up. Can we review this?”
That one call could save you from a bleeding event, a kidney injury, or a dangerous drop in blood pressure. You don’t need to be perfect. Just consistent.

King Over
Been using Medisafe for a year. Never knew how many random pills I was stacking until it flagged fish oil + aspirin. Changed my life. No drama. Just saved me from a bleed.
Johannah Lavin
OMG YES!!! 🙌 I showed my grandma this last week and she cried because she finally understood why her meds kept making her dizzy. We added all her supplements - even the ‘natural’ ones - and now she’s got a color-coded cheat sheet taped to her fridge. 🍎💊 #MedSafety
Russ Bergeman
This is the same garbage advice they give you when you’re on Medicaid. You think a free app catches interactions? I’ve seen 17 false alerts for my 8 meds. The system’s broken. Don’t trust it.
Nosipho Mbambo
I tried it... once... then got overwhelmed. There’s too many damn pills. I just assume if it’s not killing me yet, it’s fine. 😴
Ravinder Singh
Bro, you don’t need to be perfect - just consistent. Start with your top 3 meds. Add one new thing every week. I did this for my mom in India - she was on 7 pills and didn’t know st. john’s wort was canceling her antidepressant. Now she’s stable. Small steps, big wins. 💪
Ron and Gill Day
Wow. Another ‘use this app’ post. Did you even read the studies? 60% detection rate? That’s barely better than flipping a coin. This isn’t safety - it’s placebo tech for people who don’t want to talk to a real doctor.
Destiny Annamaria
I’m from the Philippines and we don’t have access to fancy apps, but my cousin in LA sent me the Liverpool checker link - saved my aunt’s life. She was on warfarin and took turmeric for ‘inflammation’ - no one told her it was like pouring gasoline on a fire. Now she only takes the checker before trying anything new. 🇵🇭❤️🇺🇸
Jeremy Samuel
lol why do people take this stuff so seriously. i just google my meds and if it dont say ‘deadly’ its fine. also ginkgo? who even uses that?
Dana Oralkhan
I used to think supplements were harmless. Then my doctor showed me how my magnesium + blood pressure med was making me dizzy. I didn’t even realize they were connected. Now I keep a little notebook. No app needed. Just awareness. You don’t need to be a tech wizard - just curious.
Alyssa Torres
I work in a pharmacy and I can’t tell you how many people come in with 10+ meds and no idea what they’re taking. One guy had 3 different painkillers, 2 sleep aids, and a ‘natural energy booster’ - all flagged red. He said ‘I thought caffeine was just coffee.’ We spent 20 minutes explaining it. He left with a printed list and tears in his eyes. This isn’t tech. This is care.
Katie Magnus
I’m a nurse. I’ve seen 3 people in the ER this month because they trusted an app over their pharmacist. One guy took 3 blood thinners because the app said ‘mild’ and he thought ‘mild’ meant ‘kinda safe.’ Spoiler: he bled out. Don’t be this guy.