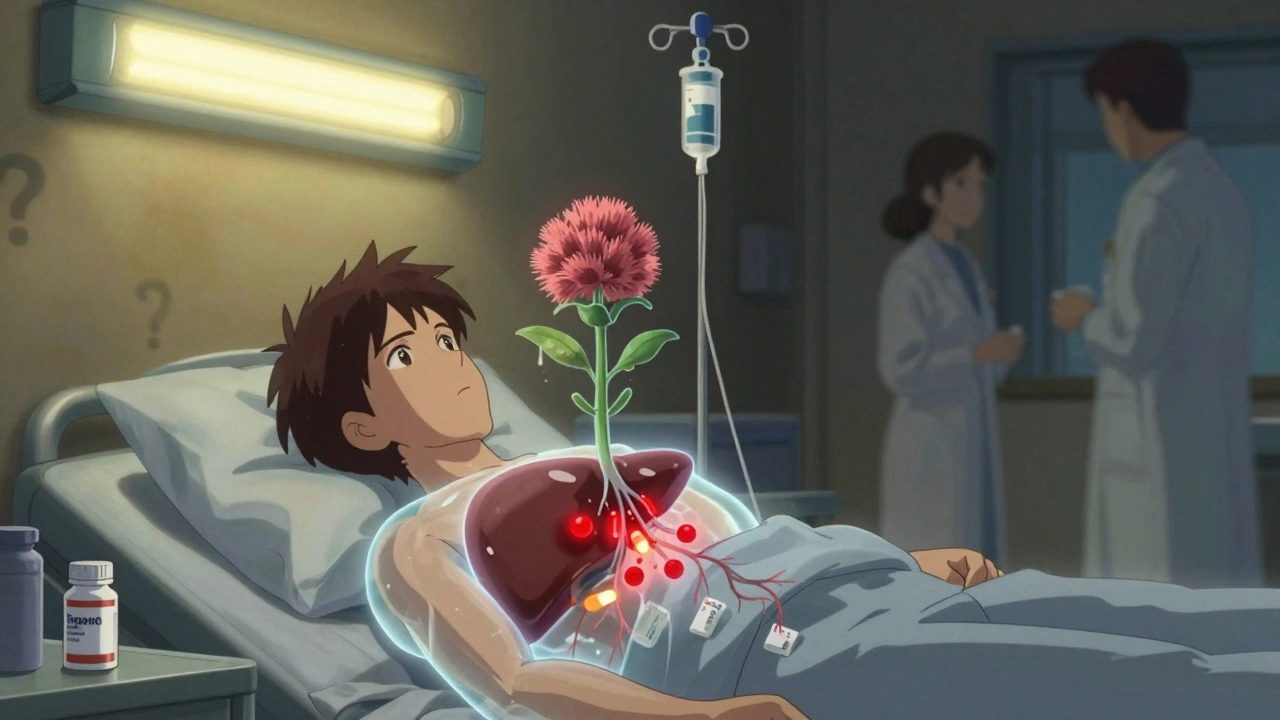
Millions of people take milk thistle every day to support liver health. It’s marketed as a natural way to detox, protect the liver, or help with fatty liver disease. But if you’re also taking medications like blood thinners, statins, or seizure drugs, you might be at risk for something you didn’t even know about: milk thistle altering how your body processes those drugs. This isn’t theoretical. Real people have ended up in the hospital because their INR levels shot up after starting a simple supplement. And it all comes down to enzymes in your liver.
How Milk Thistle Interacts With Your Liver’s Drug Processing System
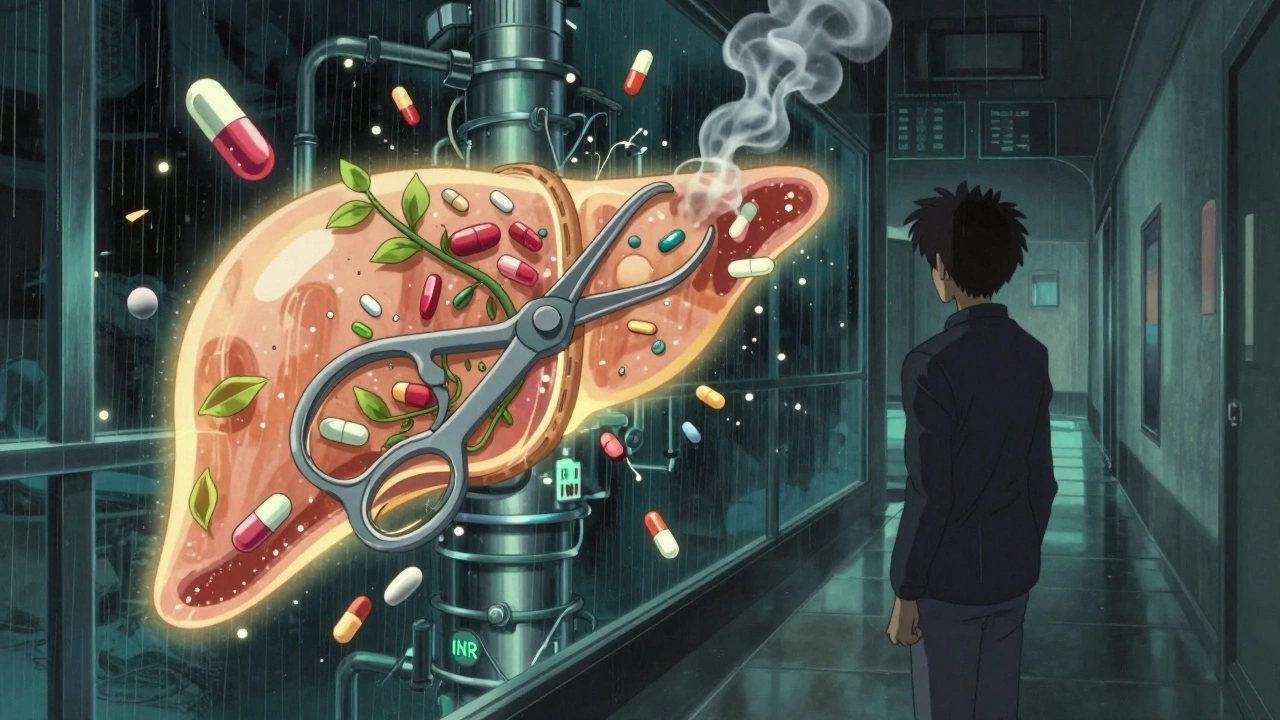
Your liver doesn’t just filter toxins. It’s also the main factory that breaks down most prescription drugs. This job is handled by a family of enzymes called cytochrome P450, or CYP enzymes. The big ones involved in drug metabolism are CYP3A4, CYP2C9, and CYP2D6. These enzymes act like molecular scissors-cutting drugs into pieces so your body can get rid of them. Milk thistle’s active ingredient, silymarin, can mess with these scissors. But here’s the twist: it doesn’t always cut slower. Sometimes it cuts faster. Sometimes it doesn’t cut at all. The effect depends on how long you’ve been taking it, how much you’re taking, and even your genes. A 2021 study showed silymarin can slow down CYP2C9 by 15-23%. That’s a problem if you’re on warfarin, a blood thinner. Slowing down this enzyme means warfarin sticks around longer. Your blood takes longer to clot. Your INR spikes. You could bleed internally without knowing it. But then a 2019 clinical trial found no real effect on CYP3A4-even at 420 mg daily for two weeks. That’s the enzyme that breaks down statins, some antidepressants, and immunosuppressants. So why do some people say their cholesterol meds stopped working after starting milk thistle? Maybe it’s not the enzyme. Maybe it’s something else. The real complication? Time. Short-term use (a few days) might inhibit enzymes. Long-term use (over a week) might actually turn them on. One study found that after 28 days, CYP2C9 activity went up by 12.7%. So if you start milk thistle and your doctor adjusts your medication after a week, you might be fine. But three weeks later? Your drug levels could crash.What Drugs Are Most at Risk?
Not all medications are equally affected. Some have a narrow window between too little and too much. These are the ones you need to watch out for:- Warfarin (Coumadin): Even small changes in metabolism can cause dangerous bleeding. There are dozens of real-world reports of INR levels jumping after milk thistle use.
- Phenytoin (Dilantin): Used for seizures. Too much can cause dizziness and confusion. Too little can trigger seizures. CYP2C9 is its main metabolizer.
- Statins (atorvastatin, simvastatin): Metabolized by CYP3A4. Theoretical risk, but clinical evidence is weak. Still, some patients report muscle pain or liver enzyme spikes after combining them.
- Immunosuppressants (cyclosporine, tacrolimus): Used after transplants. A tiny change in blood levels can mean rejection or toxicity.
- Some antidepressants and antipsychotics: Especially those processed by CYP2D6 or CYP2C9.
On the flip side, drugs like sofosbuvir/velpatasvir (hepatitis C treatments) show almost no interaction with milk thistle in clinical studies. Same with most antibiotics and painkillers like acetaminophen. The risk isn’t universal-it’s targeted.
Milk Thistle vs. Other Liver Supplements
You might be tempted to try other “natural” liver supports. But not all are created equal.- N-acetylcysteine (NAC): Works by boosting glutathione, your body’s main antioxidant. It doesn’t touch CYP enzymes. Safer if you’re on meds, but less proven for fatty liver.
- Artichoke extract: Also inhibits CYP2C9, but consistently. Less variable than milk thistle. Still, not risk-free.
- Ursodeoxycholic acid: A prescription drug for bile-related liver conditions. More effective for certain diseases, but has higher side effect rates-8.7% vs. milk thistle’s 1.2%.
Milk thistle wins on safety and tolerability. But it loses on predictability. NAC is like a steady hand. Milk thistle is like a mood swing.
Why the Confusion? Science Can’t Agree
You’ll find experts on both sides. Dr. Joseph Pizzorno, a leading voice in integrative medicine, says the risk is overstated. He points out that in 40 years of widespread use, there are only 12 documented case reports-and none proved causation. Meanwhile, Dr. David S. Bernstein, a top hepatologist, warns that without standardized extracts and consistent data, doctors should be cautious. Especially with patients on multiple drugs. The European Medicines Agency says: “No clinically relevant interactions expected.” The U.S. NIH’s LiverTox database says: “Possibly interacting with CYP2C9 substrates.” The FDA doesn’t require supplement labels to warn about drug interactions. So you’re left guessing. Even the dose matters. Most supplements contain 140-420 mg of silymarin daily. But only 32% of products on the market actually contain what’s on the label. You could be taking half the dose-or double.Real People, Real Stories
Online forums tell stories you won’t find in journals. On Reddit, a user wrote: “I started milk thistle for my fatty liver. Two weeks later, my INR jumped from 2.1 to 4.8. I almost bled out. My doctor had to cut my warfarin by 30%.” Another said: “I’ve been taking 420 mg daily for 18 months with no issues-on lisinopril, metformin, and atorvastatin.” Amazon reviews? Only 2.1% mention drug interactions. But HealthTap shows 37% of patient questions are about statins. Doctors there are split: some say “it’s fine,” others say “hold off until you check levels.” The FDA’s adverse event database has 47 reports of possible interactions between 2018 and 2023. Only 9 were confirmed. That’s low. But when you’re the one bleeding internally, 9 out of 47 doesn’t feel low.What Should You Do?
If you’re taking milk thistle and any prescription drug, here’s what actually works:- Don’t stop or start without telling your doctor. Even if you think it’s “just a supplement.”
- Know your meds. If you’re on warfarin, phenytoin, cyclosporine, or any drug with a narrow therapeutic index, assume risk until proven otherwise.
- Get tested. If you start milk thistle, ask your doctor to check drug levels (like INR, phenytoin, or tacrolimus) at day 3, day 7, and day 14.
- Wait 48 hours before baseline tests. If you’re stopping milk thistle to check drug levels, give it two days to clear. Many doctors forget this.
- Use standardized extracts. Look for products labeled “70-80% silymarin.” Avoid whole herb powders-unpredictable and untested.
- Track symptoms. Unexplained bruising, dizziness, fatigue, or muscle pain after starting milk thistle? That’s a red flag.
There’s no blanket rule. For someone with NAFLD on metformin and no other meds? Milk thistle is likely safe. For someone on warfarin, a transplant recipient, or someone taking five prescriptions? It’s a gamble.
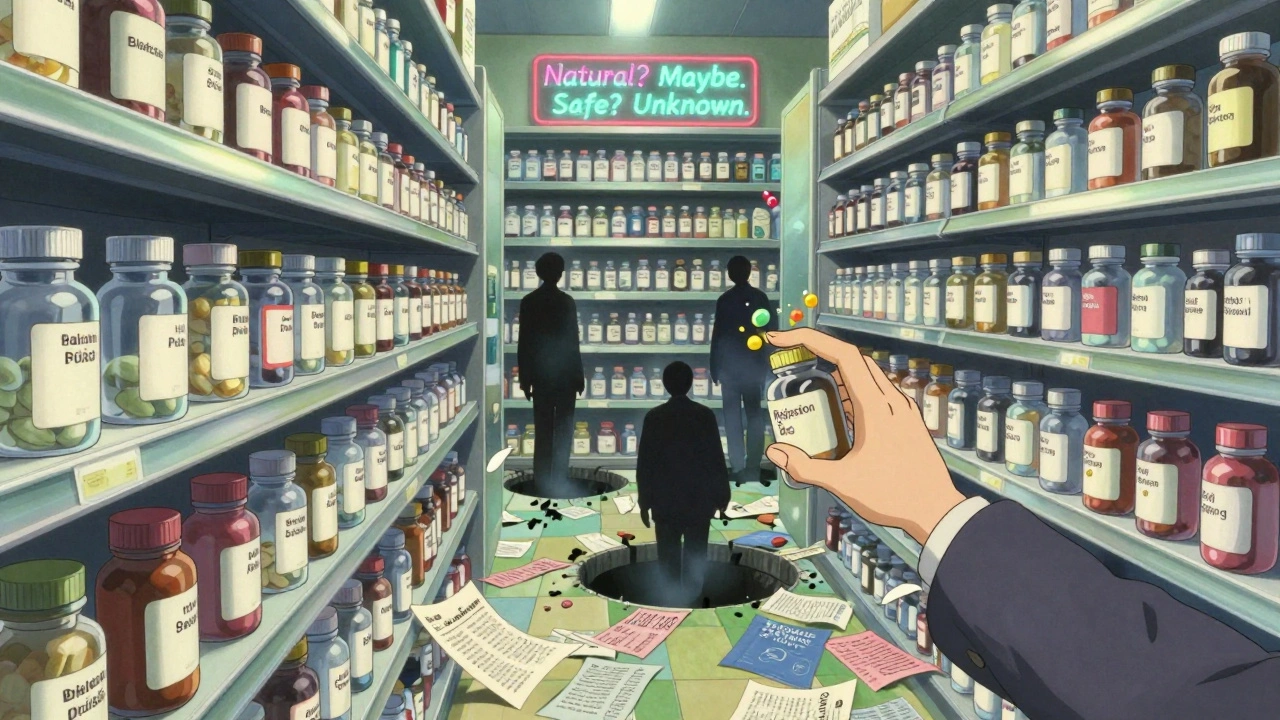
The Bigger Problem: No Labels, No Rules
Unlike prescription drugs, supplements aren’t required to test for interactions. No warning labels. No clinical data shared with doctors. The FDA only steps in if someone gets seriously hurt. That’s why 63.7% of patients ask their doctors about milk thistle-but only 28.4% of doctors feel confident answering. The knowledge gap is huge. And it’s dangerous. The market is growing fast. Milk thistle makes up nearly 40% of the global liver supplement market. But quality control? Poor. Dosing? Inconsistent. Interaction data? Incomplete. Future solutions are coming. Researchers are testing silybin bound to phosphatidylcholine-a form that may reduce CYP interactions while keeping liver benefits. But those aren’t available yet. Until then, the safest approach is simple: Assume interaction until proven safe.When Is Milk Thistle Probably Safe?
You’re probably fine if:- You’re taking it for NAFLD and only on metformin, a statin, or a blood pressure med with wide safety margins.
- You’re on a stable dose of your meds and have no history of liver or kidney issues.
- You’re not taking more than 420 mg daily.
- You’ve been on your current meds for months or years without changes.
Even then, tell your doctor. And monitor.
David Palmer
So milk thistle can mess with my blood thinner? Cool, so basically nature is just a wild card and we’re all playing Russian roulette with our meds now? 🤷♂️
Paul Dixon
I’ve been taking milk thistle for two years with statins and never had an issue, but I also get my INR checked every 4 weeks. Knowledge is power, folks. Don’t panic, just be smart.
Vivian Amadi
People still think ‘natural’ means safe? Are you kidding me? If you’re on warfarin and you take this stuff without telling your doctor, you’re not just irresponsible-you’re a walking time bomb. Stop being naive.
Jimmy Kärnfeldt
This is such a nuanced topic and I’m glad someone laid it out clearly. The fact that effects change over time-like inhibiting at first, then inducing later-is wild. Most people don’t realize supplements aren’t static. Your body adapts. So does the risk.
Ariel Nichole
Love this breakdown. I’m on cyclosporine after my transplant and I’ve been avoiding milk thistle like the plague. But I didn’t know about the time-dependent enzyme flip. That’s terrifying-and fascinating.
john damon
So like… if I take milk thistle and my statin, am I basically gambling with my muscles?? 😬 I’m gonna stop. No thanks. 🙃
matthew dendle
lol another fearmongering article about supplements. You know what causes liver damage? Alcohol. Sugar. Being fat. Not milk thistle. Stop scaring people with half-baked science
Sylvia Frenzel
Why are we even talking about this? In America we let anyone sell anything as a ‘supplement’ and then act shocked when people get hurt. This isn’t science-it’s capitalism with a side of herbal tea.
Stephanie Maillet
I’ve been thinking about this a lot lately… the idea that we treat herbs like they’re harmless, while prescription drugs are treated like sacred texts. But both are chemicals. Both interact. Both have consequences. Why do we assign moral value to ‘natural’? Is it because it feels safer? Or because we want to believe we can heal ourselves without the system? I think it’s the latter. And that’s beautiful… and dangerous.
Maybe we need to stop seeing medicine as ‘us vs. them’-natural vs. pharmaceutical-and start seeing it as ‘us vs. ignorance.’
I take milk thistle for mild fatty liver. I’m also on metformin. I told my doctor. I got my liver enzymes checked. I use a standardized 70% extract. I track how I feel. I don’t assume safety. I don’t assume danger. I just… observe.
And maybe that’s the real takeaway: not fear, not faith-but curiosity. Quiet, consistent, humble curiosity.
Because the liver doesn’t care if something is ‘natural’ or ‘synthetic.’ It only cares if it’s present. And how much. And for how long.
So ask questions. Not just of your doctor, but of yourself. Why do you take this? What are you hoping for? And are you willing to pay the price for it?
Not everyone needs to stop milk thistle. But everyone needs to understand it.
Michaux Hyatt
Biggest thing people miss: dose and duration matter more than the supplement itself. If you’re taking 140mg once a week? Probably fine. If you’re taking 420mg daily for 6 months? That’s a different story. And most people don’t even know what’s in their bottle. Get a third-party tested brand-USP or NSF certified. It’s worth the extra $5.
Also, if you’re on warfarin, get your INR checked 7 days after starting or stopping milk thistle. Don’t wait for symptoms. Bleeding doesn’t announce itself.
And if you’re a doctor? Stop dismissing supplements. Your patient isn’t stupid-they’re just trying to feel better. Meet them where they are. Guide them. Don’t judge them.
This isn’t about ‘natural vs. science.’ It’s about informed choices. And right now, most people are flying blind.