Benzodiazepines: What They Are, How They Work, and What You Need to Know
When you hear benzodiazepines, a class of central nervous system depressants used to treat anxiety, seizures, and insomnia. Also known as benzos, they work by boosting the effect of GABA, a calming neurotransmitter in your brain. This is why they help with panic attacks, muscle spasms, and trouble sleeping—but also why they carry serious risks if misused. They’re not magic pills. They’re powerful tools that can help, but they can also trap you if you’re not careful.
People often take them for short-term relief, but many end up staying on them longer than they should. That’s because your body adapts. What worked at 0.5 mg might need 1 mg after a few months, and then you’re caught in a cycle of increasing doses and withdrawal symptoms when you try to stop. Withdrawal isn’t just uncomfortable—it can be dangerous. Seizures, hallucinations, and extreme anxiety aren’t rare when people quit cold turkey. That’s why tapering under medical supervision matters more than most doctors admit.
And they don’t play nice with other meds. Mixing benzos with opioids? That’s a deadly combo—slows your breathing to a stop. Even something as simple as alcohol or sleep aids can turn a normal dose into an overdose. Some people don’t even realize they’re taking another benzo because it’s hidden in a combo pill for anxiety and depression. You need to know exactly what’s in every bottle you take.
There are dozens of types, and they’re not all the same. alprazolam, a fast-acting benzo often prescribed for panic disorder wears off quickly, which is why people take it multiple times a day—and why it’s so easy to get hooked. diazepam, a longer-acting option used for muscle spasms and alcohol withdrawal stays in your system for days, making it better for gradual tapering. Then there’s lorazepam, a middle-ground drug often used in hospitals for acute anxiety or seizures. Each has a different half-life, different risks, and different ways they interact with your liver and kidneys.
It’s not just about the drug itself—it’s about why you’re taking it. If you’re on benzos for chronic anxiety, you’re probably missing out on better long-term options like CBT or SSRIs. If you’re using them for sleep, you’re likely ignoring the root cause—stress, poor sleep hygiene, or an undiagnosed condition like sleep apnea. Benzos mask symptoms. They don’t fix problems.
And here’s the thing: most people don’t know how to talk to their doctor about stopping. They’re scared of being judged, or told they’re addicted, or that they’ll never sleep without it. But the truth is, thousands have successfully tapered off. It takes time, patience, and sometimes help from a specialist. You don’t have to stay on them forever.
Below, you’ll find real, practical guides on how to manage benzo use safely, what to watch for with other meds, how to spot dangerous interactions, and how to talk to your doctor about alternatives. No fluff. No fear-mongering. Just what you need to know to make smarter choices—whether you’re just starting out, or trying to get off.
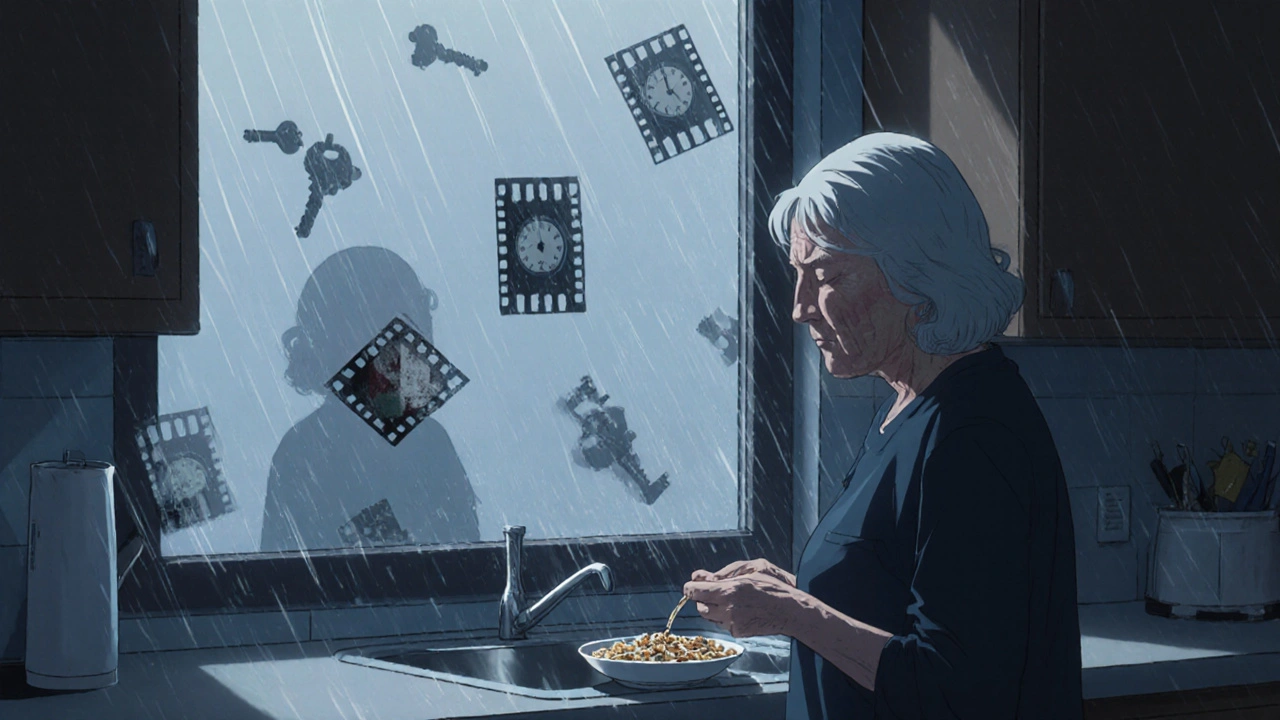
Benzodiazepines: Memory Loss, Fall Risks, and How to Taper Safely
Benzodiazepines can cause memory loss, increase fall risk in older adults, and lead to lasting cognitive issues. Learn how to taper safely and what alternatives exist.