Every year, over 30 million adults in the U.S. fill a prescription for benzodiazepines. Many take them for anxiety, insomnia, or muscle spasms. But few know the hidden costs-especially when used long-term. These drugs don’t just calm nerves. They slow down your brain. And that slowdown can stick around long after you stop taking them.
How Benzodiazepines Hurt Your Memory
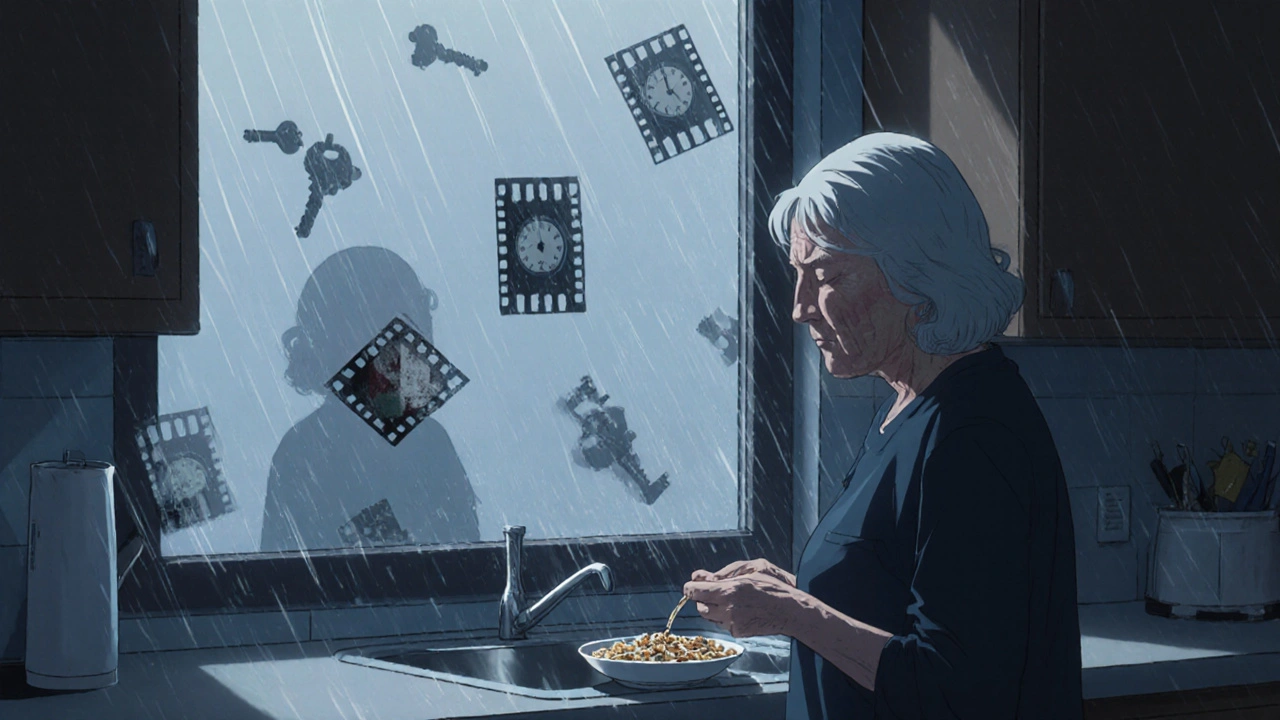
Benzodiazepines like diazepam, lorazepam, and alprazolam work by boosting GABA, a calming neurotransmitter. That’s why they help with anxiety and sleep. But that same mechanism also blocks your brain from forming new memories. This is called anterograde amnesia. You might forget what you had for breakfast, who you talked to 10 minutes ago, or where you put your keys.It’s not just occasional forgetfulness. Studies show long-term users have measurable declines in recent memory, processing speed, and executive function. One 2023 review of 19 studies found users scored significantly worse on tests measuring how quickly they could recall information, solve problems, or shift attention between tasks. The effects were strongest in people who’d been on these drugs for 10 years or more.
Even worse, these memory problems don’t vanish when you quit. A 10-month study found only 45% of former users returned to normal cognitive levels. The rest kept struggling with brain fog, slower thinking, and trouble focusing-even half a year after stopping. This isn’t normal aging. It’s drug-induced.
Falls Aren’t Just Bad Luck-They’re a Side Effect
If you’re over 65 and taking benzodiazepines, you’re 50% more likely to fall. That’s not a small risk. It’s a major danger.These drugs make you drowsy, unsteady, and slow to react. One study showed older adults on benzodiazepines had 30-40% worse balance and 25-35% slower reaction times. That’s enough to turn a minor stumble into a broken hip. In the U.S., benzodiazepines are linked to nearly 93,000 emergency room visits each year from falls in seniors alone.
Not all benzodiazepines are equal. High-potency ones like alprazolam and lorazepam are riskier than longer-acting ones like diazepam. But even the "safer" options still increase fall risk. That’s why the American Geriatrics Society has listed them as inappropriate for older adults since 2012. If you’re over 65 and still taking one, ask your doctor why.
Tapering Isn’t Optional-It’s Necessary
Stopping benzodiazepines cold turkey is dangerous. Seizures, panic attacks, hallucinations, and extreme insomnia can happen. But quitting slowly? That’s possible-and it works.The gold standard is the Ashton Protocol. Developed in the 1980s by Dr. C. Heather Ashton, it recommends reducing your dose by 5-10% every 1-2 weeks. For long-term users, that might mean cutting just 2-5% per month. The goal isn’t speed. It’s stability.
A 2021 trial with 312 long-term users showed that using diazepam (which breaks down slowly in the body) to replace other benzodiazepines made tapering smoother. At six months, 68.5% of those who followed the protocol had stopped completely. Only 27% in the control group did. And here’s the best part: cognitive improvements started within four weeks. By eight weeks, people were thinking faster and focusing better.
But it’s not easy. About 22% needed to pause their taper for a few weeks because symptoms flared up. Eight percent quit because the withdrawal felt too intense. That’s why support matters. Many people track their progress with apps like BrainBaseline. Others join online communities like the Benzodiazepine Information Coalition, where over 15,000 people share tips like "go slower than you think you need to" and "use diazepam-it’s gentler on your brain."

What Experts Say About Long-Term Use
The American Psychiatric Association says benzodiazepines should never be prescribed for more than four weeks for anxiety. Why? Because the risks outweigh the benefits after that point. The side effects aren’t just temporary. They can be lasting.Dr. Catherine Hood, director of the Benzodiazepine Research Institute, put it bluntly: "The cognitive damage from long-term use looks like early-stage dementia." That’s not hyperbole. Studies show users lose 10-15 IQ points on average. Their reaction times slow by 15-25%. Their ability to plan, organize, and speak clearly declines.
But not everyone is affected the same. Some older adults show minimal cognitive decline despite years of use. Research suggests genetics or lifestyle factors might protect some people. Still, that’s the exception-not the rule. If you’ve been on these drugs for more than a few months, assume you’re at risk.
What to Do Now
If you’re on a benzodiazepine and worried about memory or balance:- Ask your doctor for a cognitive screening. Use the MoCA or MMSE test-it’s quick and tells you where you stand.
- If your score drops by 2 points on MMSE or 3 on MoCA, it’s time to talk about tapering.
- Never stop suddenly. Work with a doctor who understands withdrawal.
- Consider switching to diazepam if you’re on a short-acting drug. It makes tapering smoother.
- Track your symptoms. Write down brain fog, memory lapses, or dizziness. You’ll see patterns.
- Give yourself time. Improvement takes months. Don’t expect overnight results.
There’s hope. People who taper successfully often report better sleep, clearer thinking, and more energy within a year. One woman in her 70s told her support group: "I forgot how to tie my shoes on this drug. Now I’m gardening again. I didn’t know I’d lost that part of myself."

What’s Next for These Drugs?
Scientists are working on new medications that target anxiety without hitting memory. Early trials of drugs that only activate specific GABA receptors (not the ones tied to memory loss) show promise. One phase II trial found a 70% reduction in anxiety-with no memory impairment. These aren’t available yet, but they’re coming.Until then, the safest choice is to avoid long-term use. If you’re already on one, you’re not alone. And you’re not broken. You just need a plan. Slow. Steady. Supported.
Can benzodiazepines cause permanent memory loss?
Benzodiazepines don’t cause structural brain damage, but they can lead to long-lasting cognitive impairments. Studies show that after stopping, 55% of long-term users still experience memory and attention problems months later. While some people recover fully, others don’t. The longer you take them, the harder it is to bounce back. That’s why early tapering matters.
Is it safe to stop benzodiazepines on my own?
No. Stopping suddenly can trigger seizures, extreme anxiety, hallucinations, or even life-threatening withdrawal. Always work with a doctor. A slow, supervised taper reduces these risks dramatically. If your doctor isn’t familiar with tapering protocols, ask for a referral to a psychiatrist or addiction specialist experienced in benzodiazepine withdrawal.
Why is diazepam often used for tapering instead of other benzodiazepines?
Diazepam has a long half-life, meaning it stays in your system longer and leaves your body more slowly. This creates a smoother withdrawal, with fewer spikes in anxiety or insomnia. Other benzodiazepines like alprazolam or lorazepam wear off quickly, causing rebound symptoms that make tapering harder. Switching to diazepam before tapering is a standard strategy recommended by experts.
How long does it take to recover cognitively after quitting benzodiazepines?
Improvement starts within weeks for many, but full recovery can take 6 to 18 months. Processing speed and attention often bounce back first. Memory and executive function take longer. One study found that 73% of people who successfully tapered reported noticeable cognitive improvement within a year. Patience and consistency are key.
Are there alternatives to benzodiazepines for anxiety or insomnia?
Yes. For anxiety, SSRIs like sertraline or escitalopram are first-line treatments with fewer long-term risks. For insomnia, CBT-I (Cognitive Behavioral Therapy for Insomnia) is more effective than sleep meds over time. Non-benzodiazepine sleep aids like suvorexant or ramelteon are also options, though they come with their own side effects. Therapy, exercise, and sleep hygiene often work better-and last longer-than pills.
Should I get my brain scanned if I’ve taken benzodiazepines long-term?
Routine brain scans (MRI, CT) aren’t needed. Research shows no permanent structural damage from benzodiazepines. The issues are functional-how your brain processes information, not its physical shape. Cognitive testing (MoCA, MMSE) is far more useful than imaging. Focus on tracking your thinking, memory, and balance instead.
Katy Bell
I was on lorazepam for 8 years for anxiety. When I finally tapered, I thought I’d feel like myself again. Turns out, I’d forgotten what ‘myself’ even looked like. Took 14 months to stop forgetting where I put my keys. Now I garden. I remember how to tie my shoes. It’s not glamorous, but it’s real.
shreyas yashas
My dad’s on diazepam for sleep. He’s 72. Last week he fell in the bathroom. Broke his wrist. Doctor said it was the meds. We’re starting the Ashton Protocol next month. I’m scared but I’m also done pretending this is normal.
Ragini Sharma
so like… i took xanax for 3 years and now i cant remember my college graduation. not even the dress i wore. is that normal? or am i just bad at life??
Manjistha Roy
Let me be clear: benzodiazepines are not a long-term solution. They are a temporary bandage on a broken bone. And if you keep using them, the bone never heals. It just gets weaker. And then one day, you fall. And you don’t get up the same.
Jennifer Skolney
I tapered off clonazepam after 10 years. First month: hell. Second month: worse. Third month: I cried because I remembered what silence felt like. Now? I sleep without pills. I think without fog. I’m not ‘cured’-but I’m me again. 💪
Olanrewaju Jeph
As a medical professional in Nigeria, I’ve seen too many patients prescribed benzodiazepines for months on end without follow-up. The cognitive decline is real, and in resource-limited settings, no one tracks it. This post should be mandatory reading for every prescriber worldwide.
Dalton Adams
Look, if you’re still on benzos after six months, you’re either in denial or you’ve never read a single peer-reviewed paper. The Ashton Protocol? That’s 1980s tech. Modern neuropharmacology has moved on. You need neuropsych testing, not ‘go slower.’ And if you’re using diazepam to taper, you’re just swapping one problem for another. The real answer is CBT-I and SSRIs. Period.
Javier Rain
My therapist said, ‘You’re not weak for needing help-you’re weak for staying on it too long.’ I cried. Then I started tapering. Four months in, I’m sleeping through the night without pills. I’m writing again. I’m laughing. This isn’t recovery-it’s resurrection.
JD Mette
I appreciate the depth of this post. The data is solid. The tone is compassionate. I’ve been off benzos for two years now. The cognitive fog lifted slowly, but it lifted. I still have moments of forgetfulness, but I’ve learned to live with them. Patience is everything.
Suresh Ramaiyan
It’s funny how we treat brain chemistry like it’s a faucet you can turn on and off. But the brain doesn’t work that way. You don’t just ‘get better’ after stopping. You rebuild. Like fixing a house while still living in it. And it’s messy. And slow. And nobody tells you that part. But it’s worth it.
Henrik Stacke
As someone who grew up in the UK where benzos were prescribed with alarming frequency in the 90s, I can confirm: the cultural normalization of these drugs has done incalculable harm. My mother was on diazepam for 22 years. She forgot my wedding. She didn’t remember my name for six months after quitting. The system failed her. We must do better.
Charmaine Barcelon
You’re all so dramatic. It’s just a pill. If you can’t handle withdrawal, maybe you weren’t meant to quit. My aunt’s on Xanax for 15 years and she’s fine. She’s happy. She’s not falling. She’s not confused. You’re making this into a crisis because you’re scared of being normal.
Karla Morales
📊 2023 meta-analysis: 55% long-term users show persistent cognitive deficits. 📉 45% return to baseline. 🧠 Diazepam taper: 68.5% success rate. 🚫 Cold turkey: 3x higher seizure risk. 📌 MoCA drop ≥3 = urgent taper. 📅 Recovery: 6–18 months. 🌱 You’re not broken. You’re just medicated. Time to un-medicate.
Kane Ren
It took me a year to feel like I could think again. But now? I read books. I write poetry. I remember birthdays. I didn’t know I’d lost those things. Thank you for this. I needed to hear I’m not alone.