Antimalarial Drugs: What They Are, How They Work, and Which Ones Actually Help
When you hear antimalarial drugs, medications designed to prevent or treat malaria, a life-threatening disease caused by parasites transmitted through mosquito bites. Also known as antimalarials, these drugs are the reason millions survive in regions where malaria is common. They’re not just pills you take before a trip—they’re a critical part of global health, especially in sub-Saharan Africa and parts of Southeast Asia. Without them, malaria would still be one of the top killers worldwide.
Not all antimalarial drugs are the same. Some, like chloroquine, a once-universal treatment for malaria that’s now ineffective in many areas due to parasite resistance, were the gold standard for decades. Others, like artemisinin, a compound derived from the sweet wormwood plant and now the backbone of modern malaria treatment, were developed because older drugs stopped working. Then there’s quinine, the original antimalarial, pulled from cinchona bark and used since the 1600s, still in use today for severe cases when newer options aren’t available. Each of these works differently—some kill the parasite in the blood, others stop it from multiplying in the liver, and some are used only in emergencies.
What’s surprising is how much resistance has changed the game. In places like Thailand and Cambodia, even artemisinin-based combinations are losing effectiveness. That’s why doctors now rely on combinations—never single drugs—to delay resistance. It’s not just about picking the right pill; it’s about using them the right way, at the right time, and in the right mix. And while prevention (like bed nets and repellents) gets more attention, antimalarial drugs are what save lives when prevention fails.
You’ll find posts here that dig into how these drugs compare, why some are cheaper than others, and how generics have made treatment possible for people who couldn’t afford brand names. You’ll see how timing, dosage, and even food can change how well they work. And you’ll learn why some drugs that once saved lives are now avoided—not because they’re dangerous, but because the parasite learned how to outsmart them.
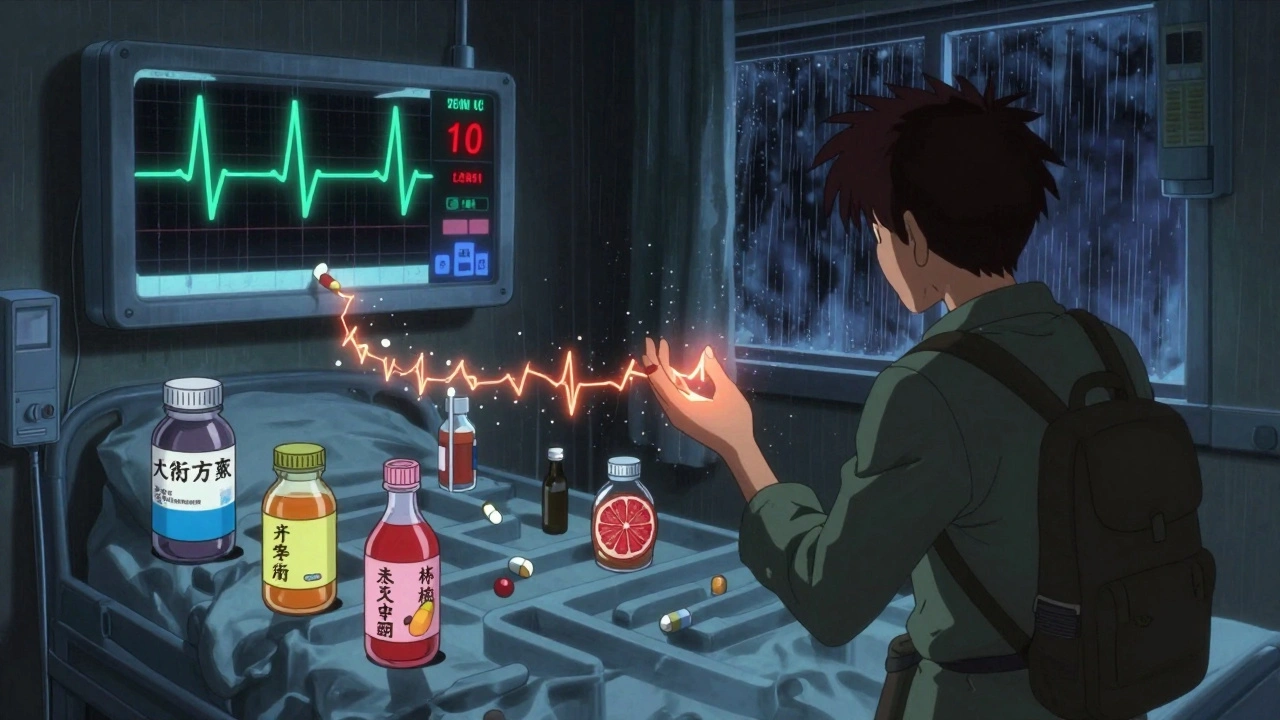
Antimalarial Medications: QT and CYP Interactions You Can't Ignore
Antimalarial drugs like hydroxychloroquine and artemether-lumefantrine can dangerously prolong the QT interval and interact with common medications through CYP enzymes. Learn which combos are deadly and how to stay safe.