When you’re prescribed selegiline transdermal (EMSAM) for depression, you might think the patch is safer than pills because it doesn’t require you to avoid cheese or red wine. But here’s the truth: the biggest danger isn’t your diet - it’s what else you’re taking. Combining EMSAM with common antidepressants, pain relievers, or even cold medicines can trigger serotonin syndrome - a life-threatening condition that spikes your body temperature, locks your muscles, and scrambles your mind. And if you’re not careful, you could end up in the ER.
How Selegiline Transdermal Works - And Why It’s Still Risky
Selegiline transdermal delivers the drug through your skin, bypassing your digestive system. This cuts down on harmful metabolites and lets you take it without strict food restrictions - but only at the lowest dose (6 mg/24 hours). Even then, it still blocks monoamine oxidase-A (MAO-A) in your brain. That’s the enzyme that breaks down serotonin. When you add another drug that boosts serotonin - like an SSRI, SNRI, or even dextromethorphan - your brain gets flooded. Too much serotonin = serotonin syndrome.
The FDA warns that EMSAM at 9 mg and 12 mg doses fully inhibits MAO-A everywhere - brain, gut, and nerves. At these levels, the risk of dangerous interactions jumps dramatically. And here’s what most people don’t realize: even if you’ve been on EMSAM for months, switching to another antidepressant isn’t as simple as stopping one and starting the other.
The Drugs That Can Trigger Serotonin Syndrome With EMSAM
You don’t need to be on a cocktail of drugs to get into trouble. Just one extra medication can be enough. The FDA lists these as absolute no-gos when using selegiline transdermal:
- SSRIs: fluoxetine, sertraline, escitalopram
- SNRIs: venlafaxine, duloxetine
- TCAs: amitriptyline, nortriptyline
- Triptans: sumatriptan, rizatriptan
- Tramadol
- Dextromethorphan
- Buspirone
- St. John’s Wort
- Tryptophan supplements
And it’s not just prescription drugs. Over-the-counter cough syrups, sleep aids, and even some herbal products can sneak in. A 2021 case report in Anesthesia & Analgesia showed a patient developed serotonin syndrome after a single dose of ondansetron - a common anti-nausea drug - while on EMSAM 9 mg. No one warned them.
Washout Periods: The 14-Day Rule Isn’t Enough
If you’re switching from an SSRI to EMSAM - or vice versa - timing matters more than you think. The FDA says you need:
- 14 days after stopping EMSAM before starting any SSRI, SNRI, or TCA
- 5 weeks after stopping fluoxetine before starting EMSAM
- 5 weeks after stopping EMSAM before starting fluoxetine
- 2 weeks after stopping other serotonergic drugs before starting EMSAM
But here’s the catch: these are the bare minimum. A 2023 study in the American Journal of Psychiatry found that MAO-A enzyme activity in the brain can take up to 28 days to fully recover after stopping EMSAM. That’s nearly a month. Many doctors still follow the old 14-day rule - but if you’ve had a bad reaction before, or if you’re older, or if you’re on other meds, you need more time.
Why does this happen? Selegiline binds to MAO enzymes permanently. Your body has to make new enzymes to replace them. That takes time - and it’s not the same for everyone. Genetic differences, liver function, age, and other drugs all affect how fast this happens.

Real Stories: When the System Failed
A 2015 study in the Journal of Clinical Psychiatry tracked 12 cases of serotonin syndrome tied to MAOIs. Three involved EMSAM. All three patients were on the 12 mg dose and had started an SSRI within days of switching. Symptoms showed up in under 72 hours - confusion, fever, shaking. One needed ICU care.
And it’s not just in hospitals. A 2023 online survey on the mental health forum Talkiatry found that 68% of 142 people prescribed EMSAM were never warned about interactions with OTC meds. Twenty-two percent had symptoms they later realized were caused by dextromethorphan in cough syrup or St. John’s Wort. One woman took a cold pill while on EMSAM and ended up in the ER with a 103°F fever and uncontrollable muscle spasms. She didn’t know it was dangerous.
Even electronic health records fail. A 2020 study found that only 43% of hospital systems flagged EMSAM-serotonin drug interactions correctly. So you can’t rely on the computer. You have to know.
What You Need to Do - Step by Step
If you’re on or thinking about EMSAM, here’s what actually works:
- Make a full list - Every prescription, OTC medicine, supplement, and herb you take. Include what you take for headaches, sleep, colds, or anxiety.
- Bring it to every appointment - Even if you’ve been on EMSAM for years. New drugs get added. Old ones get forgotten.
- Ask your pharmacist - Not just your doctor. Pharmacists have access to real-time interaction databases. Ask: “Is this safe with EMSAM?”
- Never self-switch - If you want to try a new antidepressant, don’t stop EMSAM and start something else on your own. Talk to your prescriber. Get a plan.
- Know the symptoms - Serotonin syndrome starts fast: agitation, confusion, fast heartbeat, high blood pressure, fever, muscle stiffness, tremors. If you feel this way, go to the ER. Don’t wait.
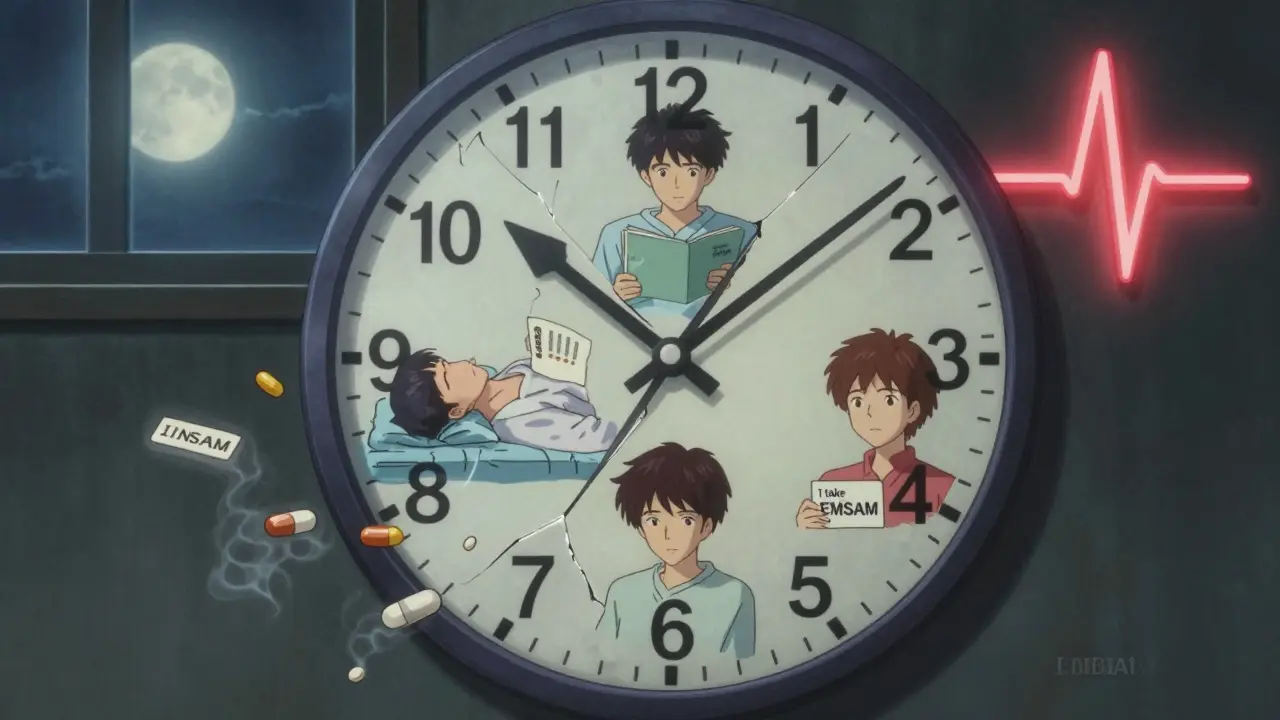
- Carry an emergency card - Write down: “I take EMSAM. Do not give me SSRIs, SNRIs, tramadol, or dextromethorphan.” Keep it in your wallet.
Why the 6 mg Patch Isn’t a Free Pass
Many patients believe that because the 6 mg EMSAM patch doesn’t require dietary changes, it’s “safe” to mix with other drugs. That’s dangerously wrong. The FDA updated its warning in May 2022 to say exactly that: “No dietary restrictions ≠ no drug interaction risks.” Even at 6 mg, EMSAM blocks serotonin breakdown in your brain. Add an SSRI? You’re still at risk.
Dr. Charles Raison, a psychiatrist at the University of Wisconsin, put it bluntly: “The idea that transdermal selegiline is ‘safer’ for drug interactions has led to preventable deaths.”
What’s Next? Better Tools Coming
Mylan, the maker of EMSAM, is developing a genetic test to predict how fast someone’s body recovers MAO enzymes after stopping the patch. Expected in 2024, this could help personalize washout times. But until then, the safest approach is simple: assume every drug you take could interact. Assume you’re at risk. Assume you need more time than you think.
EMSAM is a powerful tool for treatment-resistant depression. But it’s not a magic patch. It’s a high-stakes medication that demands respect. You wouldn’t ignore warning labels on a chainsaw. Don’t ignore them on your medicine.
Can I take ibuprofen or acetaminophen with EMSAM?
Yes, ibuprofen and acetaminophen are generally safe with EMSAM. These are not serotonergic drugs, so they don’t increase serotonin levels. However, always check with your doctor if you’re taking other medications, as some pain relievers (like tramadol) are dangerous. Stick to plain OTC pain relievers without added dextromethorphan or antihistamines.
How long does it take for EMSAM to leave my system?
The selegiline drug itself clears from your blood in hours - but the effect doesn’t. MAO enzymes are permanently blocked. It takes 2 to 4 weeks for your body to make new ones. Most guidelines say 14 days, but newer research suggests 21 to 28 days is safer, especially if you’ve been on higher doses or have liver issues.
Can I use EMSAM with anxiety meds like Xanax or Klonopin?
Benzodiazepines like alprazolam (Xanax) and clonazepam (Klonopin) are not serotonergic, so they don’t directly cause serotonin syndrome with EMSAM. However, they can mask early symptoms of serotonin toxicity (like agitation or restlessness), making it harder to spot danger. Always tell your doctor you’re on EMSAM before starting any new medication.
What if I accidentally took an SSRI while on EMSAM?
Call your doctor immediately - or go to the ER. Symptoms of serotonin syndrome can appear within hours. Do not wait. Stop the SSRI if you can, but don’t stop EMSAM yourself. Medical supervision is critical. Early treatment with serotonin blockers like cyproheptadine and supportive care can prevent serious harm.
Is there a safer MAOI than EMSAM?
No - all MAOIs carry the same core risk of serotonin syndrome. The transdermal patch reduces some risks (like dietary reactions) but not drug interactions. Other MAOIs like phenelzine or tranylcypromine require even stricter diets and have more side effects. EMSAM is the least risky MAOI available - but only if used exactly as directed.
