Every year, hundreds of thousands of people in the U.S. end up in the hospital because of drug interactions - and many of these could have been avoided simply by changing when they took their pills. It’s not always about what drugs you’re on. Sometimes, it’s about when you take them.
Why Timing Matters More Than You Think
Most people assume that if two drugs are safe to take together, the order doesn’t matter. That’s a dangerous assumption. Some interactions don’t happen because of chemistry between drugs - they happen because of timing. These are called time-dependent drug interactions (TDDIs). They occur when one drug interferes with how another is absorbed in your gut, or when stomach acid levels change too much between doses. For example, if you take ciprofloxacin (an antibiotic) at the same time as an antacid like Tums, your body might absorb less than 10% of the antibiotic. That means the infection could keep growing while you think you’re being treated. But if you wait just two hours after the antacid, absorption returns to normal. Same drugs. Different outcome. Just because of timing. The FDA estimates that 20-30% of all documented drug interactions can be prevented by spacing doses correctly. That’s not a small number. It’s a major opportunity to keep people safe without stopping any of their medications.Common Medications That Need Space Between Doses
Not all drugs play nice together - especially when taken too close. Here are the most common offenders and how to separate them:- Levothyroxine (thyroid medication) and iron or calcium supplements: Take levothyroxine on an empty stomach, first thing in the morning. Wait at least four hours before taking iron, calcium, or even a multivitamin with minerals. Studies show that if you take them together, your thyroid hormone absorption drops by up to 50%.
- Antibiotics like tetracycline or doxycycline and dairy products or antacids: Calcium in milk or yogurt binds to these antibiotics and blocks absorption. Separate by at least two hours. Same goes for antacids, iron pills, or even some fiber supplements.
- Bisphosphonates like alendronate (Fosamax): These osteoporosis drugs need to be taken with a full glass of water on an empty stomach. You must wait 30 minutes before eating, drinking anything else, or taking another pill. Otherwise, your body absorbs almost nothing.
- Proton pump inhibitors (PPIs) like omeprazole and iron supplements: PPIs reduce stomach acid, which iron needs to dissolve properly. If you take them together, you risk developing iron deficiency anemia. Space them by at least two hours - or take iron at bedtime, when you’re not taking your PPI.
- Warfarin and NSAIDs like ibuprofen: This one’s different. Timing won’t help here. Both increase bleeding risk, and the effect is cumulative. You can’t outwait this one. If you need pain relief, talk to your doctor about acetaminophen instead.
What Timing Can’t Fix
Not every interaction can be solved by waiting. Some happen inside your liver, where enzymes break down drugs. If one drug blocks the enzyme that metabolizes another, the second drug builds up to toxic levels - no matter when you take it. For example:- Warfarin + metronidazole: Metronidazole shuts down the liver enzyme that clears warfarin. This can cause dangerous bleeding. Timing won’t help. You need a dose change or a different antibiotic.
- Statins like simvastatin + grapefruit juice: Grapefruit blocks the same liver enzyme. Even one glass can cause muscle damage. No timing trick works here - you have to avoid grapefruit entirely.
- Clarithromycin + colchicine: This combo can cause fatal toxicity. The FDA recommends at least a two-hour gap, but even that isn’t always enough for older adults or those with kidney problems. Often, substitution is safer.
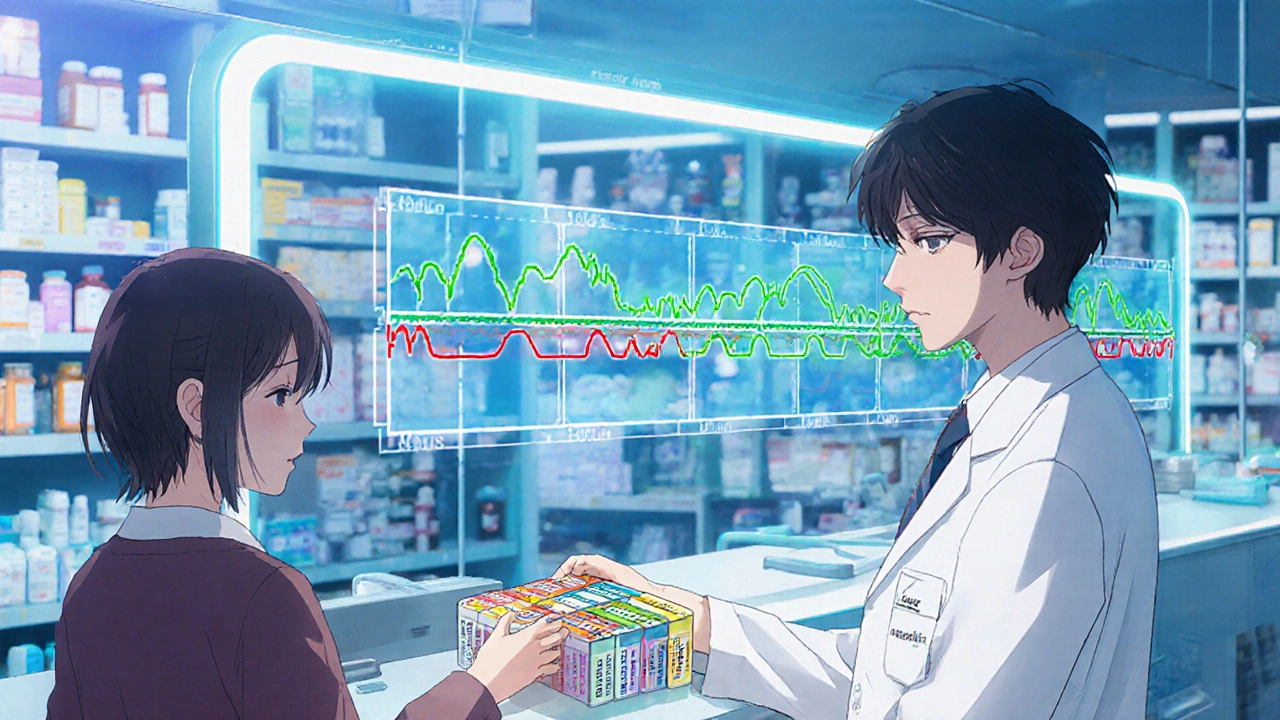
How Doctors and Pharmacies Are Getting Better at This
Ten years ago, most electronic health records didn’t warn about timing. They just flagged “possible interaction” - and left it to the patient to figure out when to space things. Now, hospitals like Kaiser Permanente and systems using Epic or Cerner have built-in alerts that say: “Give levothyroxine 4 hours before calcium.” These systems use national drug databases updated with the latest research. In 2023, 82% of U.S. hospitals had these alerts. Community pharmacies? Only 37% did. Even better, some systems now use AI to adjust timing recommendations based on your age, kidney function, or even your genetic profile. A 2024 FDA draft guidance suggests using pharmacogenomics to personalize separation times - meaning your DNA could one day tell your pharmacist exactly how long to wait between your meds.What You Can Do Right Now
You don’t need a high-tech system to protect yourself. Here’s how to start:- Make a complete list of everything you take - including vitamins, supplements, and over-the-counter drugs. Don’t forget herbal teas or magnesium supplements.
- Take it to your pharmacist. Pharmacists are trained to spot timing issues. Ask them: “Which of these need to be spaced apart?”
- Use a pill organizer with separate compartments. Buy one with morning, afternoon, evening, and bedtime slots. Label each with the time. This cuts timing errors by 43%, according to the Agency for Healthcare Research and Quality.
- Use a medication app. Apps like Medisafe or MyTherapy let you set custom alarms for each drug with notes like “Wait 4 hours before calcium.” In a 2021 study of over 1,200 patients, those using the app had 57% better adherence to timing rules.
- Write it down. If you’re on five or more meds, keep a simple chart: “Levothyroxine - 7 AM. Calcium - 2 PM. Iron - 8 PM.” Tape it to your bathroom mirror.

The Hidden Problem: Patient Confusion
Here’s the hard truth: Even when you know the right timing, it’s easy to mess up. A 2022 survey of older adults found that 68% struggled with complex schedules. Common complaints:- “I forget which meds need spacing.”
- “I took my pill at 7 AM, then my husband brought me coffee and a vitamin at 7:15. Was that too soon?”
- “I missed a dose, so I doubled up the next day - and now I feel sick.”
When to Call Your Doctor
You don’t have to figure this out alone. Call your doctor or pharmacist if:- You’re taking five or more medications.
- You’ve been diagnosed with a new condition and started a new drug.
- You feel worse after starting a new pill - even if it’s “just a supplement.”
- You’ve missed a dose and aren’t sure what to do next.
The Bigger Picture
Timing isn’t just a trick - it’s a science. And it’s one of the most underused tools in medicine. Dr. Jerry Avorn from Harvard calls it “one of the most underutilized tools in the clinician’s arsenal.” The National Academy of Medicine estimates that if we got timing right for everyone who needs it, we could prevent 115,000 to 178,000 hospitalizations each year in the U.S. That’s more than the number of people who die from opioid overdoses annually. It’s not about adding more pills. It’s about using the ones you already take more wisely. Start small. Pick one medication you’re worried about. Check with your pharmacist. Set a timer. Give it space. Your body will thank you.Can I take my blood pressure pill and my vitamin at the same time?
It depends. Most blood pressure pills are fine with vitamins. But if your vitamin contains calcium, magnesium, or iron, you may need to space them. For example, calcium can interfere with some calcium channel blockers like diltiazem. Always check with your pharmacist - don’t assume it’s safe.
What if I forget to wait the recommended time between pills?
Don’t panic. If you took two interacting meds too close together once, it’s unlikely to cause serious harm. But don’t make it a habit. One mistake won’t ruin your treatment - but repeated mistakes can lower drug effectiveness or increase side effects. Set alarms or use a pill organizer to avoid repeats.
Do I need to wait before eating after taking my thyroid medicine?
Yes. Levothyroxine should be taken on an empty stomach, at least 30-60 minutes before breakfast. Food, coffee, and even soy products can block absorption. Waiting helps your body get the full dose. If you can’t wait, take it at bedtime instead - but only if your doctor approves.
Can I use a pill organizer for all my medications?
Yes - but be careful. Some pills shouldn’t be crushed or stored for days. For example, sublingual nitroglycerin loses potency if removed from its original bottle. Always ask your pharmacist which meds are safe to put in a daily organizer. Use it for timing, not storage.
Why don’t my doctors talk about timing more often?
Many doctors are trained to focus on what drugs to prescribe, not when to take them. Pharmacists, however, are specialists in timing and interactions. If your doctor doesn’t mention it, ask: “Are there any timing rules I should follow?” Most will appreciate you being proactive.
Christina Abellar
Just started spacing my levothyroxine and calcium and I already feel less foggy. So simple, so easy to forget. Thanks for the reminder.
John Wayne
Interesting how you treat timing like some magical fix. Meanwhile, the real issue is polypharmacy. We’re overprescribing, then pretending we can outsmart the consequences with a stopwatch.
Julie Roe
I’ve been helping my mom manage her meds for years and this is the single most overlooked thing. She was taking her thyroid med with her morning coffee and a calcium gummy - no wonder her TSH was all over the place. Once we got her on a strict 7 AM pill routine with a 4-hour buffer? Her energy came back, her hair stopped falling out, and she stopped feeling like a zombie. It’s not glamorous, but it’s life-changing. I started using Medisafe and now I get little notifications for her too. If you’re juggling more than three meds, just do it. Set the alarms. Write it on your mirror. Use a pillbox with separate slots. Your body doesn’t care how busy you are - it just wants consistency. And honestly? Your pharmacist probably knows more about this than your doctor does. Don’t be shy. Walk in with your list. They’ll be thrilled you asked.
jalyssa chea
why dont doctors just give you a schedule like a school timetable like 7am thyroid 9am blood pressure 12pm ibuprofen 6pm iron 8pm ppi and then boom no more confusion why is it so hard to make it simple why do they make us guess like its a puzzle
Gary Lam
So let me get this straight - you’re telling me the secret to avoiding hospitalization is… not mixing your vitamins with your antibiotics? Wow. Next you’ll tell me not to drink bleach. I mean, I’m impressed. This is like discovering water is wet.
Peter Stephen .O
Man this hit different. I used to toss all my pills down like candy - thyroid, iron, omeprazole, you name it. Then I got dizzy, my legs cramped, and my doctor looked at me like I’d just admitted to stealing the office printer. Turned out my iron was basically just passing through me like a ghost. I started using a pill organizer with color-coded slots and set alarms labeled like ‘THYROID - NO FOOD 1HR’ and ‘IRON - WAIT 2HRS AFTER PPI’. My energy went from ‘couch potato’ to ‘hiking on weekends’. Don’t sleep on timing. It’s not just science - it’s survival. And yeah, your pharmacist? They’re the real MVPs. Bring them snacks. They deserve it.
Andrew Cairney
Wait… so you’re telling me the government and Big Pharma don’t want you to know this? 🤔 Why? Because if you spaced your meds right, you’d need fewer prescriptions, fewer lab tests, fewer hospital visits… and that means LESS PROFIT. They’re keeping you confused on purpose. I’ve seen it - my cousin’s doctor ignored her timing issues for YEARS until she ended up in ICU. Coincidence? Nah. They profit off chaos. Don’t trust the system. Take control. Write it down. Set 10 alarms. And tell everyone. This is bigger than meds - it’s about freedom.
vinod mali
i take 8 pills a day and i just started using a pill box with am pm slots. now i dont stress about missing anything. the key is just stick to one time every day. even if you sleep in, take it then. your body likes routine. also ask your pharmacist - they dont charge you for advice.
Jennie Zhu
It is imperative to underscore the clinical significance of pharmacokinetic dynamics in the context of temporal pharmacotherapy. The temporal separation of concomitant agents, particularly those exhibiting pH-dependent absorption profiles or competitive inhibition at the level of intestinal transporters, constitutes a critical intervention point in mitigating subtherapeutic exposure and iatrogenic toxicity. The empirical evidence supporting structured dosing intervals, as delineated herein, aligns with established pharmacodynamic principles and warrants integration into standardized patient education protocols.