Introduction to Carvedilol and Liver Function
As a blogger passionate about health and wellness, I often come across medications that have a significant impact on our body's vital organs. One such medication is Carvedilol, which is widely used to treat high blood pressure and heart failure. In this article, we will discuss the impact of Carvedilol on liver function, exploring its benefits, potential risks, and more. So, let's dive right in and learn more about this essential medication and its relationship with one of our most crucial organs - the liver.
Understanding the Role of the Liver in Our Body
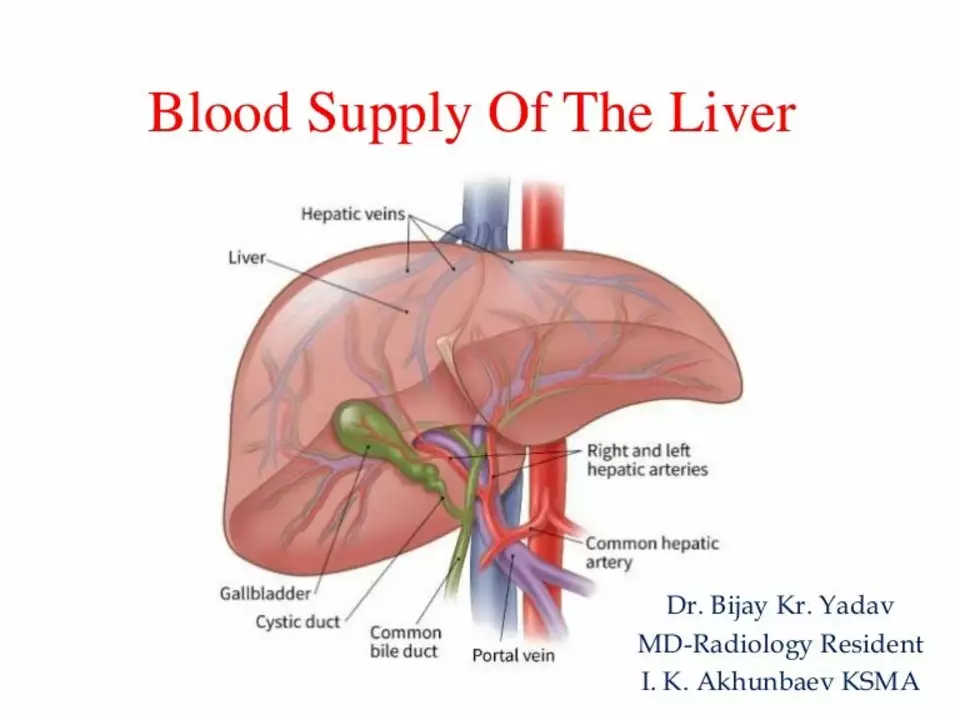
Before we delve into the impact of Carvedilol on liver function, it is essential to understand the role of the liver in our body. The liver is a large, vital organ that performs numerous functions, such as detoxification, protein synthesis, and the production of bile, which aids in digestion. It is also responsible for the metabolism of drugs and other foreign substances, which is why it plays a crucial role in the way our body processes medications like Carvedilol.
What is Carvedilol and How Does it Work?
Carvedilol is a beta-blocker medication commonly prescribed to treat high blood pressure (hypertension) and heart failure. It works by blocking the action of certain natural substances, such as adrenaline, on the heart and blood vessels. This, in turn, helps lower blood pressure, improves blood flow, and reduces the strain on the heart. While it has proven to be an effective treatment for these conditions, it is essential to understand its impact on liver function, especially for people with pre-existing liver issues.
Carvedilol and Liver Function: The Good and the Bad
Carvedilol, like any other medication, has its share of benefits and potential risks when it comes to liver function. Let's take a closer look at both sides of the coin:
Beneficial Effects of Carvedilol on Liver Function
Several studies have shown that Carvedilol can have a positive impact on liver function, particularly in patients with cirrhosis, a condition characterized by scarring and reduced liver function. Carvedilol has been found to reduce portal hypertension (high blood pressure in the liver's blood vessels) and lower the risk of serious complications like variceal bleeding in these patients. Additionally, some research suggests that Carvedilol may have antioxidant properties that can protect liver cells from damage caused by harmful substances.
Potential Risks of Carvedilol on Liver Function
On the flip side, Carvedilol has been associated with some potential risks to liver function. In rare cases, it can cause drug-induced liver injury, leading to elevated liver enzymes and, in severe cases, liver failure. This risk is higher in patients with pre-existing liver conditions, such as cirrhosis or hepatitis. It is crucial for doctors to closely monitor liver function in patients taking Carvedilol, particularly during the initial stages of treatment.
Monitoring Liver Function While on Carvedilol
Given the potential risks of Carvedilol on liver function, it is essential for healthcare providers to regularly monitor patients' liver function while they are on this medication. Blood tests, such as liver function tests (LFTs), can help detect any abnormalities in liver enzyme levels and assess the overall health of the liver. If any issues are detected, doctors may need to adjust the dose of Carvedilol or consider alternative medications to ensure the patient's liver health is not compromised.
Precautions and Tips for Taking Carvedilol
As with any medication, it is crucial to take Carvedilol as prescribed and follow your healthcare provider's advice to minimize potential risks to liver function. Some helpful tips and precautions when taking Carvedilol include:
- Inform your doctor of any pre-existing liver conditions before starting Carvedilol.
- Always take the medication as prescribed and do not make any changes to the dosage without consulting your doctor.
- Report any side effects, such as persistent nausea or vomiting, to your healthcare provider immediately, as these could be signs of liver problems.
- Maintain a healthy lifestyle, including a balanced diet and regular exercise, to support liver health and overall well-being.
Conclusion
In conclusion, Carvedilol is an effective medication for treating high blood pressure and heart failure, but it is essential to consider its impact on liver function. While it can have beneficial effects, particularly in patients with cirrhosis, it also carries potential risks, such as drug-induced liver injury. Regular monitoring of liver function and adherence to your doctor's advice are crucial to ensure optimal liver health while taking Carvedilol. Stay informed, follow a healthy lifestyle, and work closely with your healthcare provider to make the most of this essential medication.
Neeraj Agarwal
The article misspells "liver" as "livre" in one spot, but otherwise the sentences are well‑structured.
Rose K. Young
This piece is a total oversimplification of Carvedilol's risks and sounds like a lazy PR fluff piece.
Christy Pogue
Hey folks! Great rundown on how Carvedilol can both help and hurt the liver – super useful info for anyone on the meds!
Helena Pearson
While enthusiasm is welcome, we must remember that every drug carries a double‑edged sword; Carvedilol may shield portal hypertension, yet it can also tip the balance toward hepatotoxicity 😮💨🌿.
Patricia Fallbeck
Ah, the classic tale of a medication being a saviour one day and a villain the next – truly a drama worthy of a soap opera! 🎭
Brett Snyder
What a nonsense, folks! Carvedilol's benefits are far outweighing any tiny risk – any sane doctor would prescribe it without fuss.
Nidhi Jaiswal
Carvedilol can lower portal pressure but watch liver enzymes, especially if you already have liver disease.
Sunil Sharma
Exactly, regular LFT monitoring is key – it’s simple, non‑invasive, and lets doctors tweak doses before any trouble starts.
Leah Robinson
Nice summary! Keeping an eye on liver labs while on Carvedilol is a small price for the heart benefits 😊.
Abhimanyu Lala
Sure, labs are fine but remember the drug can still cause trouble – don’t just chill and ignore the signs.
Richard Sucgang
While the article is generally correct, it glosses over the rare but serious cases of liver failure induced by Carvedilol.
Russell Martin
Good point – a quick tip: if you notice persistent nausea or dark urine, flag it to your doctor right away.
Jenn Zee
In the grand tapestry of pharmacology, Carvedilol occupies a uniquely paradoxical niche, simultaneously embodying the virtues of a cardiovascular guardian and the latent perils of hepatic sabotage. First, its beta‑blocking and alpha‑blocking actions orchestrate a harmonious reduction in systemic vascular resistance, thereby attenuating the relentless onslaught of hypertension on the endothelium. Second, this hemodynamic reprieve extends to the portal venous system, where diminished pressure translates into a measurable decline in variceal bleeding risk for cirrhotic patients. Third, preclinical investigations have illuminated a modest antioxidant capacity, suggesting a protective veil over hepatocytes against oxidative stress. However, the pharmacodynamic serenity is not without its shadows; sporadic case reports have documented elevations in transaminases that, while infrequent, herald the specter of drug‑induced liver injury. Fourth, population‑based studies reveal that individuals with pre‑existing hepatic insufficiency exhibit a heightened susceptibility to these enzymatic perturbations, necessitating vigilant surveillance. Fifth, the metabolic pathway of Carvedilol, predominately hepatic via CYP2D6 and CYP2C9, introduces a variable substrate load that can overwhelm compromised livers. Sixth, dosage adjustments based on hepatic function scores have been advocated, yet real‑world adherence to such protocols remains disconcertingly low. Seventh, clinicians must balance the cardiac benefits against the hepatic risk, especially in polypharmacy scenarios where drug‑drug interactions magnify toxicity. Eighth, the therapeutic window, though broad, narrows considerably in the setting of advanced fibrosis, where even modest dosage escalations can precipitate decompensation. Ninth, emerging data suggest that genetic polymorphisms influencing beta‑blocker metabolism may further stratify risk, a frontier yet to be fully integrated into clinical practice. Tenth, patient education emerges as a pivotal pillar; an informed individual is more likely to report subtle symptoms such as fatigue or pruritus that precede laboratory derangements. Eleventh, the role of routine liver function testing cannot be overstated – a quarterly panel offers a pragmatic balance between vigilance and resource utilization. Twelfth, alternative agents, such as selective beta‑1 blockers, may confer comparable cardiac benefits with a reduced hepatic footprint, though evidence is still evolving. Thirteenth, interdisciplinary collaboration among cardiology, hepatology, and primary care is essential to navigate this therapeutic tightrope. Fourteenth, health‑system level interventions, including electronic alerts for abnormal LFTs in patients on Carvedilol, could preempt catastrophic outcomes. Finally, the clinician’s duty is to synthesize these nuanced data points into a personalized regimen that maximizes cardiovascular protection while safeguarding hepatic integrity.
don hammond
Wow, a fifteen‑sentence novel – guess some folks love to sound smart while we just need a simple ‘watch your labs’ reminder. 🙃
Ben Rudolph
Honestly, the article is fine; no need to overcomplicate what’s already clear.
Ian Banson
Fine? It downplays real risks – any serious doctor would stress stricter monitoring, not just a casual mention.
marcel lux
Appreciate the balanced view – Carvedilol does help many, but we all agree that regular check‑ups are essential.
Charlotte Shurley
Indeed, consistent monitoring aligns with best practice guidelines.
Steph Hooton
Thank you for the thorough overview; maintaining hepatic health while on Carvedilol is a shared responsibility, and your emphasis on regular testing reflects sound clinical judgment.