Pharmacists don’t just hand out pills. They’re the last line of defense against medication errors, misunderstandings, and non-adherence. But in a busy pharmacy, where the next customer is already waiting, how do you make sure every patient walks away with real understanding? That’s where pharmacist counseling scripts come in.
Why Scripts Aren’t Just Checklists
A lot of people think counseling scripts are robotic scripts you read word-for-word. That’s not how they work - and it’s not what they’re for. Scripts are training wheels. They’re the framework that helps new pharmacists cover the essentials without forgetting something critical. Think of them like a recipe: you don’t follow it exactly every time, but you need the ingredients and steps to get it right. The foundation comes from the American Society of Health-System Pharmacists (ASHP) guidelines from 1997. These guidelines didn’t just say, “Counsel patients.” They said, “You’re responsible for making sure they understand.” That’s a big shift. Before OBRA ’90, many pharmacists just offered counseling. Now, under federal law, if you’re dispensing a prescription covered by Medicaid, you’re required to actually counsel - not just offer. And it’s not just Medicaid. Most states now have their own rules. Some require you to offer counseling. Others demand you actually deliver it. California, for example, requires detailed notes on what was discussed. In 38 other states, a simple checkbox in the system is enough. That’s why scripts need to be flexible. You can’t use the same script for a 75-year-old with three chronic conditions and a 22-year-old picking up antibiotics for the first time.The Three Core Questions That Make It Work
One of the most practical frameworks comes from the Indian Health Service. It’s simple. Just three questions:- What do you know about this medication and why you’re taking it?
- How and when should you take it?
- What problems should you watch out for?
What You Must Cover (The OBRA ’90 Rules)
Federal law (OBRA ’90) says you have to talk about seven things:- The name and description of the drug
- The dosage form (tablet, liquid, inhaler, etc.)
- The route of administration (by mouth, injection, topical)
- The dosage (how much)
- The duration of therapy (how long to take it)
- Special directions and precautions (take with food? avoid alcohol?)
- Common and severe side effects
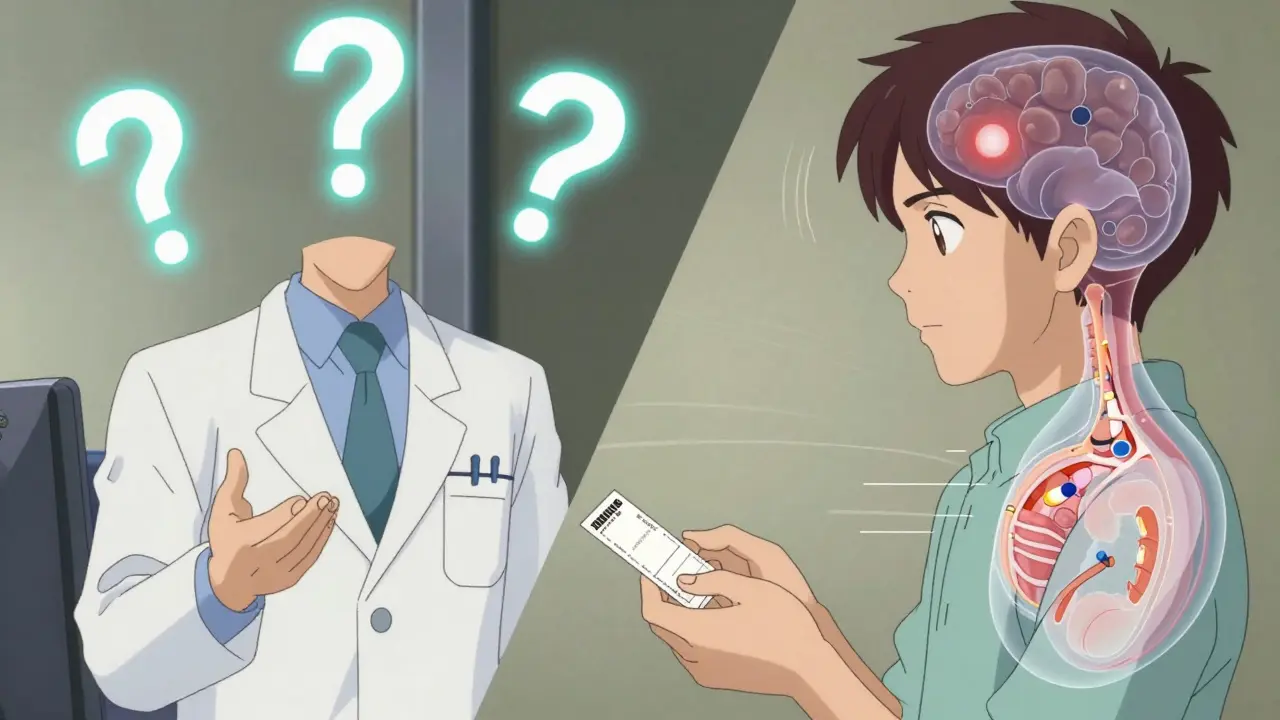
The Teach-Back Method: The Real Test of Understanding
Knowing what to say isn’t enough. You need to know if they heard it. That’s where the teach-back method comes in. Instead of asking, “Do you understand?” - which almost everyone says yes to - you ask: “Can you tell me how you’ll take this pill?” If they say, “Take one in the morning,” but the prescription says “take one with breakfast and one at bedtime,” you’ve caught a problem before it becomes a hospital visit. ASHP recommends documenting whether the patient was able to repeat the instructions in their own words. That’s not just good practice - it’s becoming a requirement. By 2025, Medicare Part D plans will need to show proof that patients understood their counseling. That means pharmacies will need to track this data.When Scripts Go Wrong
The biggest mistake? Reading them like a script. A 2019 study in the Journal of the American Pharmacists Association found that when pharmacists read scripts word-for-word, patients felt like they were being processed - not cared for. One patient said, “It sounded like a robot was telling me what to do.” Scripts should guide, not replace, conversation. Use them as a safety net, not a cage. A good pharmacist starts with the script, then listens. If the patient looks confused, they pause. If they ask a question you didn’t expect, they adapt. There’s also “script fatigue.” A 2022 survey found that 42% of pharmacists felt drained by corporate-mandated scripts that didn’t account for literacy levels, language barriers, or cultural differences. One pharmacist in Texas said her script assumed all patients could read. But 30% of her customers were Spanish-speaking and had limited English. She started using pictograms and simple translations - and adherence went up.Special Cases: Opioids, Controlled Substances, and Telehealth
Some medications need extra steps. Opioid prescriptions, for example, now require counseling on:- Proper storage (locked cabinet, out of reach of kids)
- Safe disposal (take-back programs, flushing instructions)
- Naloxone availability - and how to use it

Documentation: It’s Not Optional
You can’t counsel without documenting. ASHP says you need to record:- That counseling was offered
- That it was accepted (or refused)
- What was covered
- Whether the patient demonstrated understanding
How to Get Started
If you’re new to counseling:- Learn the OBRA ’90 seven-point checklist cold.
- Practice the three-question framework with a colleague.
- Use the teach-back method on every patient - even if you think they get it.
- Start documenting everything, even if your pharmacy doesn’t require it yet.
- Watch experienced pharmacists. Notice how they pause, rephrase, and ask follow-ups.
What’s Next for Counseling Scripts
The future is dynamic. Pilot programs at CVS and Walgreens are testing AI-powered scripts that adjust in real time. If a patient says, “I get dizzy when I take this,” the system suggests adding a warning about orthostatic hypotension. If they ask, “Can I drink coffee?” it pulls up interaction data. These tools don’t replace pharmacists. They make them better. In early trials, patient comprehension scores jumped 23%. And the economic reason is clear: medication non-adherence costs the U.S. $312 billion a year. Every dollar spent on good counseling saves $5 in avoided hospital visits. Counseling isn’t a box to check. It’s the reason pharmacists are trusted. And with the right scripts - used the right way - it’s something every pharmacist can do well.Are pharmacist counseling scripts required by law?
Yes, under OBRA ’90, pharmacists must counsel patients on Medicaid-covered prescriptions. Many states have gone further and require counseling for all prescriptions. While federal law mandates offering counseling, 18 states require actual counseling to be delivered, not just offered. Documentation of counseling is also legally required in most states.
What’s the difference between ASHP and CMS counseling guidelines?
ASHP guidelines focus on best practices for pharmaceutical care - emphasizing patient-centered communication and comprehensive education. CMS guidelines are more regulatory, focused on compliance with OBRA ’90 and Medicare Part D requirements. ASHP gives you the “why,” CMS gives you the “what you must do.” Most pharmacies use both: ASHP for training, CMS for documentation.
Can I use the same script for every patient?
No. A good script is a framework, not a script. A 70-year-old with diabetes and high blood pressure needs different details than a teenager on birth control. Adjust based on age, literacy, language, health conditions, and the medication. The three-question framework helps you tailor it - don’t read it verbatim.
How do I handle language barriers during counseling?
Use professional interpreter services - not family members. Many pharmacies use telephonic interpretation (like Language Access Network) that supports over 150 languages. Always provide written materials in the patient’s language. Never rely on Google Translate. Studies show patients who receive counseling in their native language are 50% more likely to take medications correctly.
Why is the teach-back method so important?
Because “Do you understand?” gets a fake yes. Teach-back asks patients to explain it in their own words. If they say, “I take this when I feel sick,” but it’s meant for daily use, you catch a dangerous misunderstanding. It’s the only reliable way to confirm comprehension - and it’s becoming a requirement for Medicare Part D plans by 2025.
Do I need special training to use counseling scripts?
Yes. Most pharmacy schools require 8-12 weeks of supervised counseling practice. The American Society of Consultant Pharmacists recommends 15 hours of continuing education per year on communication skills. Scripts are tools - but using them well takes practice, feedback, and reflection. Don’t skip training.
What’s the biggest mistake pharmacists make with counseling?
Reading the script like a robot. Patients notice when you’re not listening. The goal isn’t to check a box - it’s to build trust. Use the script to guide your conversation, not replace it. Listen more than you talk. Ask open-ended questions. Let the patient lead when they can.
Meina Taiwo
Just worked a 12-hour shift at a community pharmacy in Lagos. The three-question framework works wonders. Patients who can’t read English? Use pictures. One guy thought his blood pressure pill was for headaches. We drew a heart and a tablet. He got it. No script needed-just clarity.
Sarah Williams
This is the stuff that actually saves lives. Not the checkboxes. Not the corporate compliance forms. The real talk. The teach-back. The pause. The look in their eyes when they finally get it. Do this right, and people don’t just take their meds-they trust you.
Erika Putri Aldana
LOL so now pharmacists are therapists? 😂 Next they’ll make us fill out a mood tracker with our prescriptions. I swear, if I have to listen to one more robot voice say ‘take with food’ I’m switching to CVS.
Grace Rehman
They call it counseling but it’s really just compliance theater wrapped in buzzwords
OBRA ’90 was a start but now it’s变成了 a paperwork circus
And don’t even get me started on AI scripts that don’t know what ‘cultural humility’ means
People aren’t data points. They’re humans with stories. And no algorithm can replace a pharmacist who actually listens
Jerry Peterson
I’ve seen pharmacists in rural Kentucky do this right. No script. Just a smile, a pause, and ‘So what’s your plan for taking this?’
They didn’t need fancy tech. Just time. And respect.
That’s what’s missing now.
Orlando Marquez Jr
While the structural framework presented herein is methodologically sound, it remains critically deficient in its ontological alignment with contemporary patient autonomy paradigms. The three-question heuristic, though pragmatic, implicitly assumes a hierarchical epistemic relationship between provider and patient, thereby undermining the foundational tenets of shared decision-making as codified in the Belmont Report. Furthermore, the reliance on standardized protocols risks reifying biomedical hegemony at the expense of phenomenological lived experience. A truly patient-centered model would require epistemic humility, not templated scripts.
Sandy Crux
Oh, brilliant. Let’s turn every pharmacist into a corporate-trained parrot reciting OBRA’s gospel. And let’s not forget the ‘teach-back’ method-because nothing says ‘I care’ like forcing a confused elderly woman to repeat medical jargon in front of a line of 12 people. Also, AI scripts? How quaint. Next, they’ll replace pharmacists with chatbots that say ‘Take with food’ in 17 languages while ignoring the fact that half the patients don’t eat food-they eat canned beans and sugar water. Truly, innovation.
Dan Adkins
India developed this three-question model decades ago. We didn’t need AI or corporate compliance to teach people how to take medicine. We had community health workers, respect for elders, and the understanding that knowledge isn’t owned by institutions-it’s shared. Now the West wants to patent it, monetize it, and turn it into a checklist. You didn’t discover this. You just stole it. And now you’re charging for it.
Theo Newbold
Let’s analyze the data. 38 states require a checkbox. 18 require actual counseling. 92% of documentation is boilerplate. 42% of pharmacists report script fatigue. The correlation between mandatory scripts and patient adherence is r=0.18. The ROI on counseling is $5 saved per $1 spent-but only if the counseling is documented correctly. And here’s the kicker: 67% of those documentation entries are copied from prior visits. So we’re spending billions on a system that’s mostly performative. The real problem isn’t the script. It’s the system.
Peggy Adams
Wait… so now the government’s making pharmacists do ‘teach-back’ because they don’t trust patients to read the label? And AI is gonna fix it? LOL. I bet the same people who made this also think ‘take with food’ means ‘take with a bag of chips.’ This whole thing is a scam. They just want to bill more. And the worst part? They’re gonna make us pay for it with higher co-pays.
Adrian Thompson
OBRA ’90 was a Trojan horse. First, they made you counsel. Then they made you document. Then they made you use EHRs. Then they made you use AI scripts. Next thing you know, the FDA’s gonna send bots to your pharmacy to audit your tone. They don’t want you to help patients. They want you to be a data-gathering node for Big Pharma. And don’t even get me started on ‘naloxone availability’-that’s just a backdoor to push opioid regulation under the guise of ‘safety.’
Sarah Williams
Just saw a pharmacist at my local CVS use the three-question method with a guy who didn’t speak English. Used a phone interpreter, showed him the pill bottle, and asked him to point to when he’d take it. He pointed to breakfast and bedtime. Perfect. No script. Just human. That’s what this is really about.