Peripheral artery disease, or PAD, isn’t just about leg pain. It’s a warning sign your whole body is at risk. When arteries in your legs, arms, or neck get clogged with plaque, blood flow slows down-and that’s when trouble starts. About 8.5 million Americans have PAD, and most don’t even know it. If you’re over 65, smoke, have diabetes, or high blood pressure, you’re in the high-risk group. Left untreated, PAD doesn’t just make walking painful. It raises your chance of heart attack or stroke by 3 to 5 times. The good news? If caught early, you can stop it from getting worse-and even feel better without surgery.
What Does PAD Actually Feel Like?
Not everyone with PAD feels symptoms right away. In fact, up to 40% of people with confirmed PAD have no noticeable signs. But when symptoms do show up, they’re hard to ignore. The most common one is claudication-cramping, aching, or tiredness in your calves, thighs, or hips that comes on when you walk and goes away when you rest. It’s not just being out of shape. This pain is predictable: same distance, same time, same feeling. Walk a block, stop. Walk another block, stop again. That’s claudication.
As PAD gets worse, symptoms get more serious. You might feel pain in your feet or toes even when you’re sitting still-especially at night. This is called rest pain, and it means your tissues aren’t getting enough oxygen. Your skin may turn pale or bluish. Toenails thicken and stop growing. Hair falls off your legs. Your feet feel cold, even in warm rooms. Sores on your toes or heels won’t heal. If you’re a man, erectile dysfunction can be an early clue-up to 75% of men with PAD report this issue.
These aren’t random changes. They’re signs your body is starving for blood. The same plaque that blocks leg arteries is likely clogging arteries in your heart and brain. That’s why PAD isn’t just a leg problem-it’s a red flag for your entire cardiovascular system.
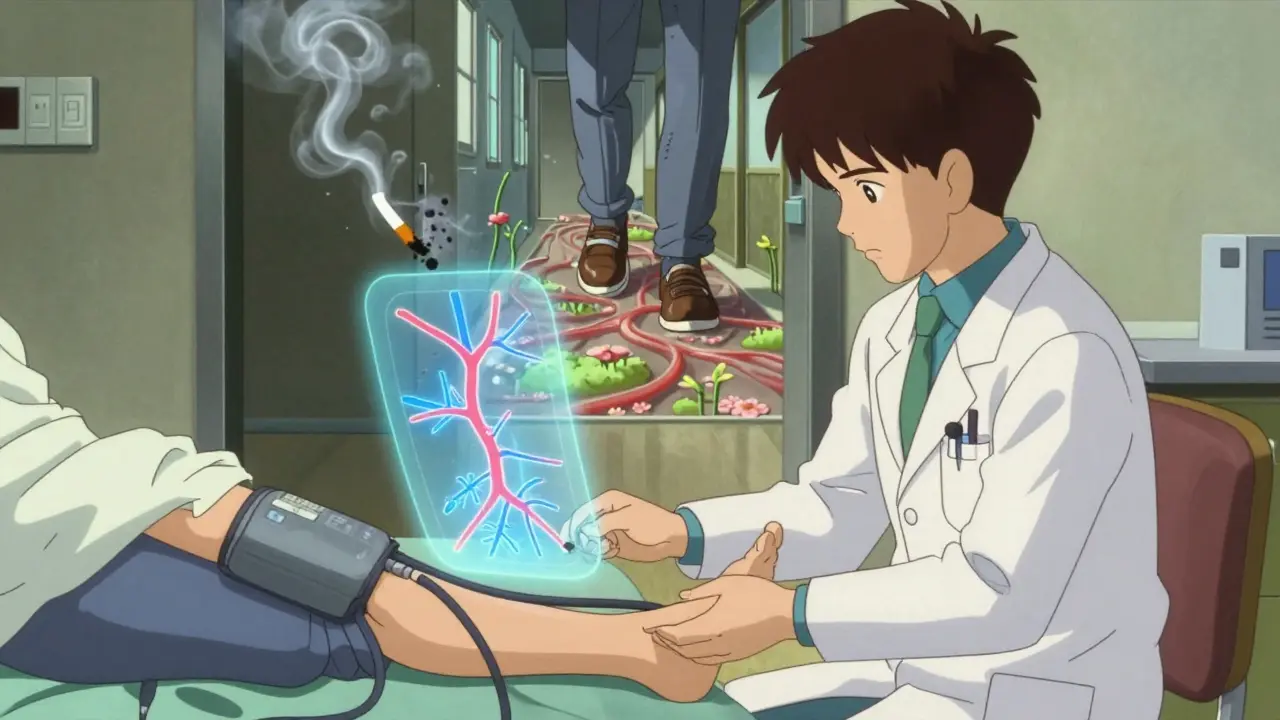
How Do Doctors Diagnose PAD?
Diagnosing PAD starts with a simple test: the ankle-brachial index, or ABI. It’s non-invasive, quick, and cheap. Your doctor measures your blood pressure in both arms and both ankles. Then they compare the numbers. If the pressure in your ankle is less than 90% of the pressure in your arm, you have PAD. An ABI of 0.90 or lower confirms it. Values below 0.40 mean severe disease.
But ABI isn’t perfect. If you have diabetes or kidney disease, your arteries can become stiff and hard to compress. In those cases, doctors use the toe-brachial index (TBI). If your toe pressure is below 0.70 compared to your arm, you likely have PAD.
Ultrasound is the next step. It shows exactly where the blockage is and how bad it is. No needles, no radiation. Just sound waves mapping your blood flow. For more detail, doctors may order a CT angiogram or MRI angiogram. These give 3D images of your arteries and show blockages down to the millimeter. The most accurate test is catheter angiography-where a thin tube is threaded into your artery and dye is injected. But it’s invasive, so it’s usually saved for when surgery is being considered.
Screening isn’t just for people with symptoms. The American Heart Association recommends ABI testing for everyone over 65. If you’re 50 or older and smoke or have diabetes, get tested. If you’re 40+ with multiple risk factors-high cholesterol, high blood pressure, obesity-don’t wait for pain to start.
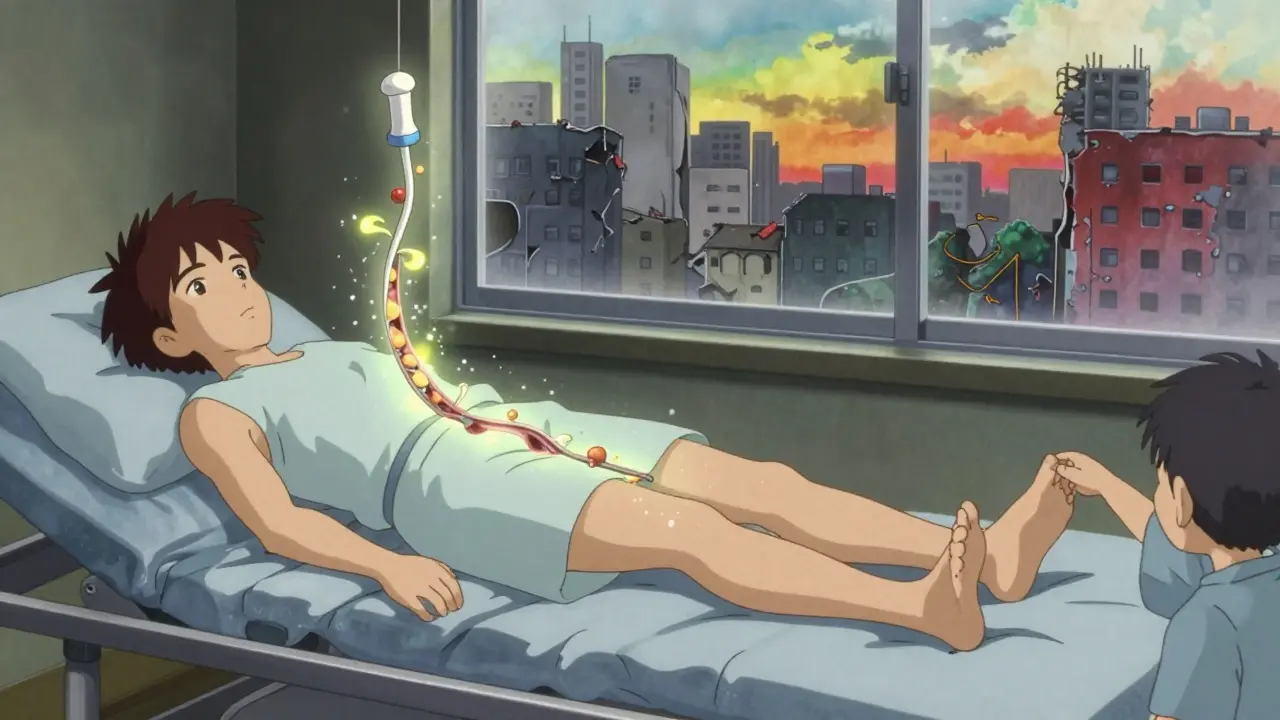
What Happens If You Don’t Treat PAD?
PAD doesn’t go away on its own. Without treatment, it gets worse. The blockages grow. Blood flow drops. Tissues begin to die. That’s when you enter the danger zone: critical limb ischemia. At this stage, you might have sores that won’t heal, blackened skin (gangrene), or constant pain that keeps you awake at night. Without surgery, about half of these patients lose a foot or leg within a year.
But amputation isn’t the biggest risk. The real danger is what’s happening inside your heart and brain. PAD patients have a 30-40% chance of dying within five years-similar to many cancers. Most don’t die from a blocked leg artery. They die from a heart attack or stroke caused by the same plaque that’s clogging their legs.
And here’s the scary part: only 20% of people who should be screened for PAD actually are. Many doctors don’t check. Many patients ignore the pain, thinking it’s just aging or arthritis. But PAD is not normal. It’s a medical emergency waiting to happen.
Lifestyle Changes: The First Line of Defense
Before any medication or surgery, the most powerful tool you have is your own behavior. And the two biggest things you can do? Quit smoking and start walking.
Smoking is the #1 cause of PAD progression. If you keep smoking, your risk of amputation goes up 8 times. Your chance of dying from heart disease triples. Quitting isn’t just helpful-it’s life-saving. Even if you’ve smoked for decades, quitting now cuts your risk dramatically.
Walking is the best medicine for claudication. Not just any walking-structured, supervised walking. A program of 30 to 45 minutes, three to five times a week, for at least 12 weeks, can double your walking distance. You walk until the pain hits, rest until it goes away, then walk again. Repeat. This trains your body to use oxygen better, builds new tiny blood vessels, and reduces pain over time. Studies show people who stick with it can walk 150-200% farther without pain.
Other changes matter too. Eat less saturated fat. Control your blood sugar if you’re diabetic. Keep your blood pressure under 130/80. Lose weight if you’re overweight. These aren’t just “good habits.” They’re medical treatments that directly slow plaque buildup.
Medications That Actually Work
If lifestyle changes aren’t enough, medications step in. There are three main types that make a real difference.
First, antiplatelets. These thin your blood just enough to stop clots from forming in narrowed arteries. Aspirin (81 mg daily) is common. But clopidogrel (75 mg daily) works better-it cuts heart attacks, strokes, and death by 20.5% compared to aspirin in PAD patients, based on the CAPRIE trial.
Second, statins. Everyone with PAD needs one, no exceptions. Even if your cholesterol is normal. Statins don’t just lower LDL-they stabilize plaque, reduce inflammation, and cut cardiovascular events by 25-30%. The goal? Get your LDL below 70 mg/dL. That’s not a suggestion. It’s the standard.
Third, cilostazol. This is the only pill specifically approved to treat claudication. It improves blood flow and can increase walking distance by 50-100%. But it’s not for everyone. If you have heart failure, avoid it. Side effects include headaches and palpitations. But for those who can take it, it’s a game-changer.
Other drugs like blood pressure meds or diabetes meds are used too-but only if you need them. The key is taking the right pills, consistently. Skipping doses makes them useless.
When Surgery or Procedures Are Needed
If pain limits your life and meds aren’t enough, it’s time to consider reopening the blocked arteries. There are several options, all less scary than they sound.
Angioplasty is the most common. A tiny balloon is threaded into the blocked artery and inflated to flatten the plaque. Often, a stent-a small metal mesh tube-is left behind to keep the artery open. Success rates are high: 90% for short blockages. Recovery is quick: often just one night in the hospital.
Atherectomy is used when plaque is hard and calcified. A tiny rotating blade or laser shaves the plaque away. It’s especially helpful for patients with diabetes or kidney disease, where arteries are more brittle.
Bypass surgery is for longer, more complex blockages. A vein from your leg (or a synthetic tube) is grafted around the blocked section. It’s major surgery, but it lasts. Vein grafts stay open 80% of the time after five years.
Here’s the catch: surgery doesn’t replace lifestyle changes. If you keep smoking or eat poorly after a stent, the artery can clog again. These procedures fix the blockage-but only you can stop the cause.
What’s New in PAD Treatment?
Research is moving fast. One big study, VOYAGER PAD, found that adding a blood thinner called rivaroxaban (2.5 mg twice daily) to aspirin reduced the risk of limb complications and heart events by 15% in patients after revascularization. This combo is now being used more often.
Stem cell therapy is still experimental, but early results are promising. In trials, injecting a patient’s own stem cells into their leg muscles helped heal wounds in 65% of cases-compared to 35% with standard care. It’s not standard yet, but it’s coming.
Imaging is getting smarter, too. Optical coherence tomography (OCT) lets doctors see plaque in microscopic detail during procedures. This helps them place stents more precisely and avoid complications.
And finally, policy is catching up. The PAD Awareness Act of 2022 gave $5 million a year to fund free screening programs in high-risk communities. Starting in 2024, clinics and pharmacies in underserved areas will offer free ABI tests. This could change everything for people who never thought they needed to get checked.
What Should You Do Next?
If you’re over 50 and smoke, or over 65, or have diabetes-get an ABI test. It takes five minutes. It costs less than a coffee. It could save your leg, your heart, or your life.
If you already have PAD, don’t wait. Start walking today. Quit smoking. Take your meds. See your doctor regularly. PAD isn’t a death sentence. It’s a call to action. And the earlier you act, the better your odds.
The numbers don’t lie: 30-40% of PAD patients die within five years. But those who manage their condition-through walking, quitting smoking, and taking their meds-live longer, walk farther, and avoid amputations. You have more control than you think.
Can peripheral artery disease be reversed?
Yes, in many cases. While plaque doesn’t vanish completely, lifestyle changes and medications can stop it from growing and even shrink it slightly. Walking regularly, quitting smoking, lowering LDL cholesterol below 70 mg/dL, and controlling blood pressure can stabilize the disease and improve blood flow. Some patients see their walking distance double within months. The goal isn’t to erase the plaque-it’s to prevent it from causing damage.
Is leg pain always a sign of PAD?
No. Leg pain can come from nerve issues, arthritis, muscle strain, or spinal problems. But PAD pain is specific: it happens during activity, stops with rest, and returns predictably. If your pain is constant, burning, or tingling, it’s more likely nerve-related. If it’s cramping that comes and goes with walking, get checked for PAD.
Can I still walk if I have PAD?
Yes-and you should. Walking is the most effective treatment for claudication. Start slow. Walk until the pain begins, rest until it fades, then walk again. Repeat for 30-45 minutes. Over time, your body adapts. Many people find they can walk farther without pain after just 12 weeks. Avoiding movement makes PAD worse.
Does PAD only affect the legs?
Mostly, yes. PAD most commonly affects arteries in the legs. But it can also occur in the arms, kidneys, stomach, or neck. If you have PAD in your legs, you likely have plaque buildup elsewhere too. That’s why it’s a marker for heart attack and stroke risk. Your whole vascular system is at play.
How often should I get checked if I have PAD?
If you’ve been diagnosed, see your doctor every 3 to 6 months. They’ll check your ABI, blood pressure, cholesterol, and foot health. If you’re on medication, they’ll monitor for side effects. If you’re not improving, they may refer you to a vascular specialist. Don’t wait for symptoms to return-regular checkups prevent emergencies.
What If You’re Not Getting Better?
If you’re doing everything right-walking, quitting smoking, taking meds-but your pain is getting worse or wounds aren’t healing, it’s time to see a vascular specialist. Not a general doctor. Not a podiatrist. A vascular surgeon or interventional radiologist who specializes in PAD.
They can offer advanced options: newer stents, drug-coated balloons, atherectomy devices, or even clinical trials for stem cell therapy. You might also need a foot care team to manage ulcers and prevent infection.
And if you’re struggling to quit smoking or stick to a walking routine, ask for help. Many hospitals offer free smoking cessation programs and supervised exercise programs for PAD patients. You don’t have to do this alone.
PAD is serious. But it’s not hopeless. The tools to beat it exist. The question is: will you use them?

Jody Patrick
PAD is just another government scam to sell statins. They don't want you walking because that's free. They want you on pills forever. Look at the data - 80% of 'PAD cases' are just lazy people who won't get off the couch.
Radhika M
If you have diabetes or smoke, walk every day - even just 10 minutes. It helps more than medicine. Your legs will thank you. No need to wait for a test. Start now.
Philippa Skiadopoulou
The clinical evidence supporting ABI screening in asymptomatic individuals remains inconclusive. While the American Heart Association recommends it, the USPSTF has not endorsed universal screening due to insufficient data on long-term outcomes and cost-effectiveness.
Pawan Chaudhary
You got this. I used to walk only 2 blocks before my legs gave out. Now I walk 2 miles. Took 4 months. Took effort. But I’m alive and pain-free. You can too. Just start today. One step.
Jonathan Morris
Notice how the article never mentions that the pharmaceutical industry funds 92% of PAD research. Cilostazol? Rivaroxaban? All patented drugs with 10x markup. The real solution? Stop eating processed food. But that doesn't sell ads or pills. They want you dependent. Watch your local pharmacy's profit margins - they're rising faster than your LDL.
Linda Caldwell
Walk. Just walk. Not tomorrow. Not next week. NOW. Your legs are screaming for blood. You don’t need a doctor to tell you that. You need to move. One block. Then another. Then ten. You’re not broken. You’re just asleep. Wake up. Your life is waiting.
Anna Giakoumakatou
How quaint. A 12-week walking program is the new yoga. We’ve replaced enlightenment with endothelial function. Tell me, does your cilostazol come with a gratitude journal? Or is that sold separately, next to your $400 statin?
CAROL MUTISO
It’s funny how we treat PAD like a mechanical problem - clogged pipes, pills, procedures - when it’s really a spiritual one. We’ve forgotten how to listen to our bodies because we’re too busy optimizing our lives for productivity. Walking isn’t therapy. It’s rebellion. Quitting smoking isn’t health. It’s reclaiming your autonomy from a system that wants you docile, medicated, and distracted. The plaque? It’s not just in your arteries. It’s in our culture.
Erik J
Has anyone studied the correlation between ABI scores and long-term cognitive decline? I’m wondering if reduced cerebral perfusion from systemic atherosclerosis plays a role in early dementia. The paper I read last year suggested a link, but the sample size was small.
BETH VON KAUFFMANN
It’s concerning that the article conflates correlation with causation regarding smoking and PAD progression. The 8x amputation risk figure is from a 2003 cohort study with significant confounding variables - including socioeconomic status, access to care, and comorbidities. Also, the CAPRIE trial’s 20.5% reduction is relative risk, not absolute. The NNT is 44. You’re better off investing in a good pair of walking shoes than chasing pharmacological miracles.