When your legs ache after walking just a few blocks, it’s easy to blame aging, bad shoes, or being out of shape. But if that pain comes back every time you walk, fades when you rest, and feels like cramping or heaviness in your calves, thighs, or hips-you could be dealing with something more serious: peripheral artery disease. It’s not just about tired legs. PAD is a warning sign that your arteries are clogged, not just in your legs, but possibly everywhere in your body. And that raises your risk of heart attack and stroke-just as much as having diabetes or high blood pressure.
What Exactly Is Peripheral Artery Disease?
Peripheral artery disease, or PAD, happens when fatty deposits build up in the arteries that carry blood to your arms, legs, or feet. This buildup-called atherosclerosis-is the same process that causes heart attacks. But instead of blocking blood to the heart, it’s blocking blood to your limbs. The result? Not enough oxygen gets to your muscles when you’re active, which triggers pain, cramping, or fatigue.
It’s more common than most people think. About 8.5 million Americans have PAD, and nearly 1 in 5 people over 65 are affected. Yet, most don’t know it. Only about 20% of people who should be screened actually get tested. That’s dangerous because PAD doesn’t just hurt your legs-it’s a red flag for your heart. People with PAD are 3 to 5 times more likely to have a heart attack or stroke than those without it.
Classic Symptoms: It’s Not Just “Getting Older”
The most well-known sign of PAD is claudication-pain in your legs that shows up when you walk and goes away when you stop. It’s not a dull ache. It’s a tight, crampy, burning feeling in your calves, thighs, or buttocks. After walking a certain distance-maybe 5 minutes or 2 blocks-the pain hits. Rest for 10 minutes, and it’s gone. Repeat the next day, same thing.
But not everyone has this classic symptom. About half of people with PAD feel no pain at all. That’s why it’s often missed. Other signs include:
- Cool skin on your feet or legs compared to the rest of your body
- Weak or absent pulses in your feet
- Shiny, thin skin on your lower legs
- Loss of hair on your shins or feet
- Slow-growing or thickened toenails
- Sores on your toes, feet, or legs that won’t heal
- Pain in your legs even when you’re resting-especially at night
- Erectile dysfunction in men, which can be one of the earliest signs
If you notice any of these, especially if you’re over 50, smoke, have diabetes, or have high blood pressure or cholesterol, don’t ignore them. These aren’t normal signs of aging. They’re signs your body isn’t getting enough blood.
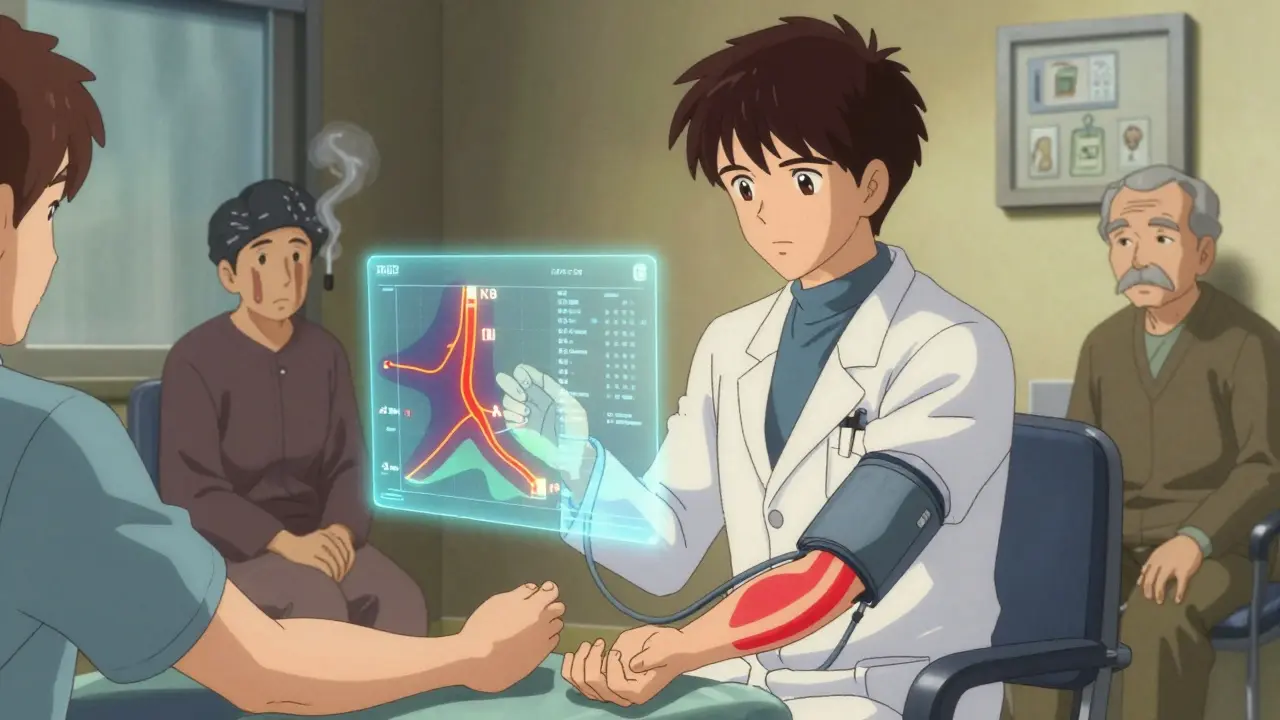
How Doctors Diagnose PAD
Diagnosing PAD is straightforward-but only if your doctor thinks to check. The first test is usually the ankle-brachial index, or ABI. It’s a simple, painless test that compares the blood pressure in your ankle to the blood pressure in your arm. If the ankle pressure is significantly lower, it means blood flow is blocked somewhere down there.
An ABI of 0.90 or below confirms PAD. If it’s below 0.40, the blockage is severe. For people with stiff arteries-common in diabetics or kidney disease patients-the toe-brachial index (TBI) is used instead. A TBI below 0.70 signals trouble.
If the ABI suggests PAD, doctors often follow up with a Doppler ultrasound. This uses sound waves to see how blood is moving through your arteries and where blockages are. For more detail, they might use a CT angiogram or MRI angiogram. These create 3D pictures of your arteries and show exactly where and how badly they’re narrowed.
Only in rare cases, when surgery is being considered, do doctors use traditional angiography-a catheter inserted into the artery with dye to see blockages in real time. It’s accurate, but it’s invasive and carries small risks like kidney damage from the dye.
The American Heart Association recommends ABI screening for:
- Everyone 65 and older
- Anyone 50 or older who smokes or has diabetes
- Anyone 40 or older with multiple heart disease risk factors
If you fit any of these groups and haven’t been tested, ask your doctor. It takes less than 10 minutes and could save your leg-or your life.
Treatment: It’s Not Just About the Legs
Treating PAD isn’t just about relieving leg pain. The real goal is to keep you from having a heart attack or stroke. That means tackling the root cause: atherosclerosis.
Lifestyle Changes: The First and Most Important Step
Walking. Not running. Not biking. Walking. A supervised walking program-30 to 45 minutes, 3 to 5 days a week-can double or even triple how far you can walk without pain. It works because it forces your body to grow new tiny blood vessels around the blockages. Over 12 weeks, most people see big improvements.
Quitting smoking is even more critical. If you keep smoking, your risk of needing an amputation goes up 8 times. Your chance of dying from heart disease triples. No other single change makes more difference.
Medications: Protecting Your Heart and Limbs
Most people with PAD need at least two types of medications:
- Antiplatelets: Aspirin (81 mg daily) or clopidogrel (75 mg daily). Clopidogrel is slightly more effective at preventing heart attacks and strokes in PAD patients.
- Statins: These lower cholesterol and stabilize plaque. Doctors aim for LDL cholesterol below 70 mg/dL. Studies show statins cut heart events by 25-30% in PAD patients.
- Cilostazol: This drug helps improve walking distance by 50-100%. It’s not for everyone-people with heart failure shouldn’t take it.
High blood pressure and diabetes also need tight control. Keeping your blood pressure under 130/80 and your HbA1c under 7% reduces complications significantly.
Procedures: When Medications Aren’t Enough
If pain limits your daily life and doesn’t improve with meds and walking, doctors may recommend a procedure to open the blocked artery.
- Angioplasty: A tiny balloon is inflated inside the artery to crush the blockage. Works well for short blockages-success rate around 90%.
- Stents: A metal mesh tube is left in place to keep the artery open. About 80% stay open after one year.
- Atherectomy: A device shaves away the plaque. Best for hard, calcified blockages.
- Bypass surgery: A vein from your leg or a synthetic tube is used to reroute blood around the blockage. The saphenous vein graft lasts 5 years or more in 80% of cases.
Costs vary. A walking program costs about $1,200. Angioplasty runs $15,000-$25,000. Bypass surgery can hit $30,000-$40,000. But none of these compare to the cost of an amputation or a heart attack.
Why Early Detection Matters More Than You Think
PAD is a silent killer. The 5-year death rate for people with PAD is 30-40%. That’s higher than many types of cancer. Most of those deaths are from heart attacks or strokes-not leg problems.
Even more troubling: Black and Hispanic patients are 30-40% less likely to get revascularization procedures than white patients, even when their disease is just as bad. That’s not just unfair-it’s deadly.
The PAD Awareness Act of 2022 started funding screening programs in high-risk communities. But until more people know the signs, and until doctors make screening routine, too many will be left behind.

What’s Next for PAD Treatment?
Research is moving fast. The VOYAGER PAD trial showed that adding a blood thinner called rivaroxaban to aspirin reduced the risk of limb events by 15% in patients who’d had a procedure. That’s now part of new guidelines.
Stem cell therapies are being tested for critical limb ischemia. In early trials, 65% of patients saw improved wound healing after receiving their own stem cells. That’s promising for people with non-healing ulcers who’ve run out of options.
Advanced imaging like optical coherence tomography (OCT) lets doctors see plaque at a microscopic level. That could mean more precise treatments in the future-fewer repeat procedures, better outcomes.
But none of this matters if you don’t know you have it. If you’re over 50, smoke, have diabetes, or have leg pain when you walk-get tested. It’s simple. It’s quick. And it could change everything.
Can peripheral artery disease be reversed?
Yes, in many cases. While the plaque buildup doesn’t disappear completely, lifestyle changes-especially walking and quitting smoking-can stop it from getting worse and even improve blood flow. Medications like statins stabilize the plaque so it’s less likely to rupture. In some patients, symptoms improve so much they can walk without pain again. The key is early action.
Is PAD the same as varicose veins?
No. Varicose veins are swollen, twisted veins near the skin’s surface caused by weak valves. They’re mostly a cosmetic issue, though they can cause discomfort. PAD is about blocked arteries deep in the legs, reducing blood flow to muscles. One affects veins, the other arteries. One is usually harmless; the other is life-threatening.
Does PAD only affect the legs?
Mostly, yes. But PAD is a sign of widespread atherosclerosis. If your leg arteries are blocked, so are likely your heart arteries, brain arteries, and kidney arteries. That’s why PAD patients have such high risks of heart attack and stroke. It’s not just a leg problem-it’s a full-body warning.
Can I still exercise if I have PAD?
Yes-and you should. Walking through the pain, as uncomfortable as it is, is one of the best treatments. It trains your body to grow new small blood vessels that bypass the blockages. Start slow, walk until the pain hits, rest until it goes away, then walk again. Do this 3-5 times a week. Within weeks, you’ll notice you can walk farther without pain.
What happens if PAD is left untreated?
Without treatment, PAD can progress to critical limb ischemia-where pain happens even at rest, and sores don’t heal. This can lead to infection, gangrene, and amputation. Even worse, the risk of heart attack or stroke skyrockets. Up to 40% of people with untreated PAD die within 5 years. Early detection and treatment can cut that risk in half.
Are there any natural remedies for PAD?
No natural remedy has been proven to treat or reverse PAD. Supplements like garlic, ginkgo, or omega-3s may help general heart health, but they don’t replace proven treatments like walking, quitting smoking, statins, or antiplatelets. Relying on supplements alone can delay care and lead to serious complications.
What to Do Next
If you’re over 50 and have any risk factors-smoking, diabetes, high blood pressure, or leg pain when walking-ask your doctor for an ABI test. It’s free or low-cost in most clinics. Don’t wait for pain to get worse. Don’t assume it’s just aging. PAD is treatable, but only if caught early.
If you already have PAD, stick with your walking plan, take your meds, and quit smoking. Your legs will thank you. But more importantly, your heart will too.
Jody Patrick
PAD is just the government’s way to scare old folks into buying more meds. Walk more? Quit smoking? That’s not medicine, that’s moralizing.
Radhika M
If you are over 50 and walk slow because legs hurt, get ABI test. It is cheap, easy, and can save your life. No need to wait for pain to get worse.
Philippa Skiadopoulou
The clinical evidence supporting ABI screening in asymptomatic populations remains inconsistent. While lifestyle modification is universally beneficial, overdiagnosis leads to unnecessary interventions and patient anxiety.
Pawan Chaudhary
You got this! Even if you’re just walking around the block at first, every step counts. Your body’s smarter than you think - it’ll thank you later.
Jonathan Morris
They never mention that 70% of PAD cases are diagnosed post-amputation. The system waits until you’re crippled before it cares. This isn’t medicine - it’s triage capitalism.
Linda Caldwell
Walk through the pain. Seriously. I did it. Started at 2 blocks, now I do 3 miles. No magic pills. Just boots on the ground and showing up every day. You can too.
Anna Giakoumakatou
Oh, so now we’re supposed to believe that walking is the cure? How quaint. Did the pharmaceutical lobby fund this article too? Or is this just another wellness cult pitch wrapped in medical jargon?
CAROL MUTISO
It’s wild how we treat arteries like they’re plumbing - fix the clog, and everything’s fine. But the real issue? We’ve built a society that rewards silence over suffering. PAD doesn’t scream. It whispers. And we’ve trained ourselves not to listen.
That’s why the real treatment isn’t statins or angioplasty - it’s learning to hear your body before it breaks. And then, actually doing something about it. Not just for you, but for the people who never get tested because they don’t have insurance, or time, or hope.
I’ve seen patients cry because they thought their pain was ‘just old age.’ They weren’t lazy. They were invisible.
So yeah - walk. Quit smoking. Take your meds. But also - ask your doctor for the ABI. Push for it. If you’re lucky enough to have access, don’t let someone else’s neglect become your tragedy.
Erik J
Is there data on how many people with ABI < 0.90 actually progress to critical limb ischemia without intervention? I’m curious about the natural history curve.
BETH VON KAUFFMANN
Let’s be clear: the entire PAD paradigm is a monetized surveillance apparatus. ABI testing is a gateway to statin prescriptions, then antiplatelets, then angioplasty - all while the root cause - systemic inflammation from ultra-processed foods - remains unaddressed. This is vascular capitalism at its finest.
Martin Spedding
my doc said i had pad but i dont feel that bad?? maybe its just my shoes??
Raven C
How dare you reduce the profound, systemic tragedy of arterial decay to a checklist of lifestyle modifications? You speak of walking as if it were a prayer - as if the soul of the body could be healed by mere repetition. The arteries do not forgive. They do not forget. And neither should we.
And yet… you still don’t understand. This isn’t about your legs. It’s about the slow, silent betrayal of the body by a civilization that values productivity over presence. You walk because you’re told to - not because you feel the weight of your own mortality.
Perhaps you should sit. And listen. Not to your calves - to your silence.