Heart disease kills more women than all forms of cancer combined. Yet, many women still believe stroke or breast cancer is their biggest threat. The truth? Heart disease is the number one killer of women in the U.S. and around the world. Every year, about 307,000 women die from it - that’s one in five female deaths. But here’s the problem: most women don’t recognize the signs. And when they do, doctors often miss them too.
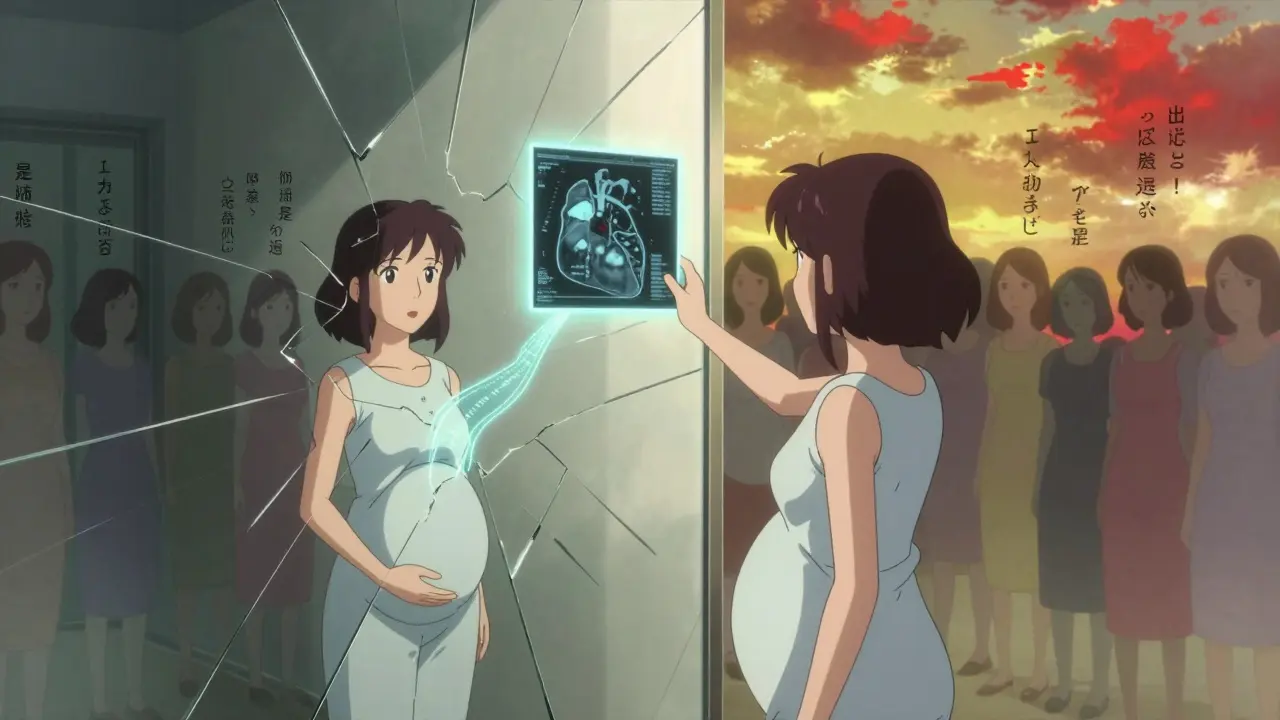
What Makes Women’s Heart Disease Different?
For decades, heart disease research focused almost entirely on men. The famous Framingham Heart Study, started in 1948, enrolled only men. That shaped how doctors learned to spot heart problems - and it left women behind. Today, we know women’s hearts behave differently. Their arteries are smaller. Their symptoms don’t always look like the classic chest-crushing movie scene. And their risk factors? They’re not the same.Women are more likely to develop conditions like microvascular disease - where the tiny blood vessels in the heart get damaged - rather than the large artery blockages men typically get. They’re also far more likely to experience spontaneous coronary artery dissection (SCAD), a tear in a heart artery that can happen without warning, often in women under 50 with no other risk factors. Then there’s Takotsubo syndrome, also called broken heart syndrome, which is triggered by extreme stress and hits women nine times more often than men.
Symptoms Women Don’t Talk About - But Should
Most people picture a heart attack as intense chest pain, gripping the arm, collapsing. But for women, that’s only part of the story. In fact, nearly half of women who have heart attacks never feel chest pain at all.Here’s what women actually report - and what doctors too often overlook:
- Unexplained fatigue - not just being tired, but exhaustion so deep it makes you unable to make your bed or walk to the mailbox. This happens in 71% of women after a heart attack.
- Shortness of breath - not during a workout, but while doing normal things like walking to the kitchen or talking on the phone.
- Jaw, neck, or back pain - especially on the left side. It might feel like a toothache or a pulled muscle, but it doesn’t go away with rest.
- Nausea, vomiting, or indigestion - many women think they’ve eaten something bad. In reality, it’s their heart sending distress signals.
- Dizziness or lightheadedness - sudden, unexplained, with or without sweating.
- Sleep disturbances - waking up gasping, or feeling unusually tired even after a full night’s sleep.
One study found that women are 59% more likely than men to mistake these symptoms for stress, anxiety, or aging. And that delay? It costs lives. On average, women wait 2.3 hours longer than men to call 911. By then, heart muscle is already dying.
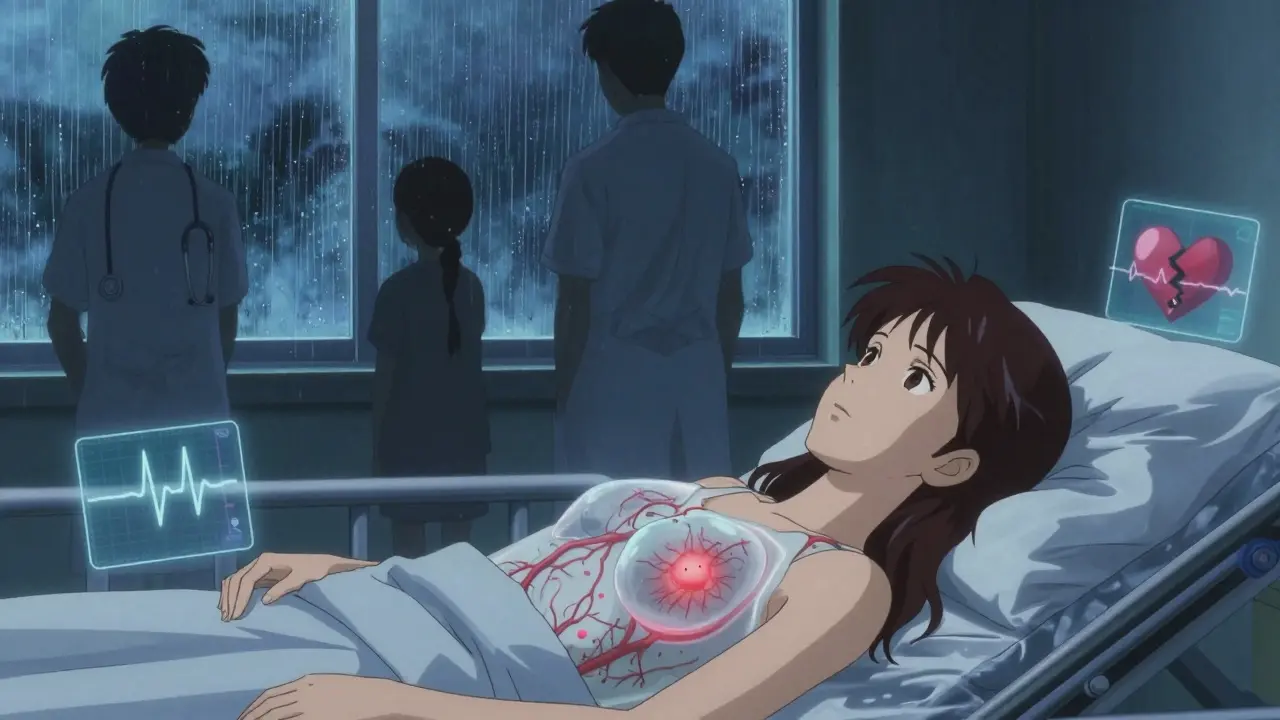
Why Diagnosis Is So Often Wrong
Emergency rooms are filled with women sent home because their EKG looks normal or their troponin levels are “just a little off.” But standard tests were designed on male bodies. A woman’s heart attack doesn’t always show up on an EKG the same way. Her blood markers rise slower. Her symptoms come on gradually, not like a sledgehammer.And then there’s bias. A 2022 study in JAMA Internal Medicine found that 68% of women with cardiac symptoms were dismissed as anxious, stressed, or hormonal. One woman described being told, “You’re just going through menopause,” while her heart was failing. Another was sent home with antacids - three times - before she finally had a massive heart attack.
Women under 55 are seven times more likely than men to be sent home from the ER without proper testing. And within a year, those misdiagnosed women have a 50% higher chance of dying.

Hidden Risk Factors Only Women Face
High cholesterol and smoking matter for everyone. But for women, some risks are unique:- Pregnancy complications - preeclampsia, gestational diabetes, or delivering a baby under 3.5 pounds raises future heart disease risk by 80%.
- Early menopause - before age 45 - doubles the risk of coronary artery disease.
- Polycystic ovary syndrome (PCOS) - linked to insulin resistance, high blood pressure, and unhealthy cholesterol levels.
- Autoimmune diseases - lupus, rheumatoid arthritis, and others increase inflammation that damages arteries.
- Mental stress - women are 37% more likely than men to have angina triggered by emotional stress. Grief, caregiving, work pressure - these aren’t just emotional burdens. They’re cardiac risks.
Many women don’t realize their history matters. If you had a baby with preeclampsia 15 years ago? You’re not just “fine.” You’re at higher risk - and you need to talk to your doctor about it.
What Women Should Do - Right Now
The good news? You can protect yourself. Here’s what works:- Know your numbers - Blood pressure, cholesterol, blood sugar. Don’t wait for your annual checkup. Ask for them every year. If you’re over 40, ask about a coronary calcium scan - it can spot early artery buildup before symptoms appear.
- Track your symptoms - Keep a journal. Note when you feel unusually tired, short of breath, or have unexplained pain. Bring it to your doctor. Say: “I’ve had this for two weeks. Could it be my heart?”
- Don’t ignore fatigue - If you’re exhausted for more than two weeks, especially if it’s worse than usual and paired with shortness of breath, get checked. This is one of the most common warning signs in women.
- Find a women’s heart program - Hospitals with specialized cardiac care for women have 22% higher survival rates after heart attacks. Ask if your hospital has a Women’s Cardiovascular Center of Excellence. As of 2023, there are 147 certified centers across the U.S.
- Ask about new tests - The Corus CAD test, approved in 2020, analyzes gene expression to detect heart disease in women with 88% accuracy - far better than traditional stress tests.
What’s Changing - And What’s Still Broken
There’s progress. The NHLBI launched the RENEW initiative in 2023, pouring $150 million into research on women’s heart health. The FDA approved gender-specific diagnostic tools. And public campaigns like Go Red for Women have helped more women recognize the signs.But gaps remain. Only 34% of cardiovascular research funding targets women’s specific needs. Women make up 51% of the U.S. population, but only 38% of participants in heart studies. And insurance companies still don’t always cover tests that work better for women.
The goal? By 2030, the American Heart Association wants 70% of women to know heart disease is their biggest threat. Right now, it’s 44%. We’re not there yet.
When to Act - Not Wait
If you’re a woman and you experience three or more of these symptoms - fatigue, shortness of breath, nausea, jaw pain, back pain, or dizziness - don’t wait. Don’t assume it’s stress. Don’t call your friend first. Call 911. Or go to the ER. Say: “I think this might be my heart.” If they hesitate, ask: “Can you rule out a heart attack with a coronary calcium scan or the Corus CAD test?”Heart disease doesn’t announce itself with a siren. For women, it whispers. And if you’re not listening - or if your doctor isn’t either - the consequences are deadly.
Do women have heart attacks without chest pain?
Yes. About 43% of women who have heart attacks don’t feel chest pain at all. Instead, they may have extreme fatigue, nausea, shortness of breath, back or jaw pain, or dizziness. These are not "atypical" - they’re typical for women. Ignoring them because there’s no "classic" chest pain can be fatal.
Can pregnancy affect my heart health later?
Absolutely. Complications like preeclampsia, gestational diabetes, or preterm delivery raise your risk of heart disease by up to 80% later in life. Even if you feel fine after pregnancy, you should discuss your history with your doctor. These are not just pregnancy issues - they’re warning signs for future heart problems.
Is heart disease only a concern for older women?
No. While heart disease risk increases with age, women under 50 are increasingly affected. Conditions like SCAD and Takotsubo syndrome often strike younger women - even those who are active and healthy. Don’t assume you’re too young. If you have symptoms, get checked.
Why are women misdiagnosed more often than men?
Because symptoms are different and doctors are trained on male-centric data. Studies show 68% of women with cardiac symptoms are incorrectly labeled as anxious, stressed, or hormonal. The system was built for men. Women’s hearts don’t fit that mold - and that gap costs lives.
What tests should women ask for?
Ask for a coronary calcium scan if you’re over 40 with risk factors. If you have symptoms but standard tests are normal, ask about the Corus CAD test - it’s validated specifically for women and is 88% accurate. Also request a stress echo or cardiac MRI if microvascular disease is suspected. Don’t accept a negative EKG as proof you’re fine.
Can lifestyle changes really reduce my risk?
Yes - but not just diet and exercise. Managing stress, getting enough sleep, and controlling inflammation matter just as much. Quitting smoking cuts risk by half. Walking 30 minutes a day lowers blood pressure and improves circulation. And if you have PCOS, preeclampsia, or early menopause, work with a cardiologist who understands these links - not just a general practitioner.
Are there any new treatments for women’s heart disease?
Yes. Beyond gender-specific diagnostic tools like Corus CAD, hospitals with Women’s Cardiovascular Centers of Excellence now use protocols designed for women’s physiology. These include faster testing, lower thresholds for intervention, and team-based care that avoids dismissal of symptoms. AI tools trained on female symptom patterns are also emerging and could cut misdiagnosis by up to 40% in the next five years.
Heart disease doesn’t care if you’re busy, strong, or young. It doesn’t care if you’re the caregiver, the mother, the worker, the leader. It waits. And if you don’t listen - or if the system doesn’t listen for you - it takes you. The data is clear. The tools exist. The question is: will you act before it’s too late?
Ernie Simsek
Bro, I had a heart attack and didn't even feel chest pain. Just felt like I'd been run over by a truck after a 3am shift. Went to the ER, got sent home with Tums. Three days later, I collapsed. Don't be a statistic. 🤯
Joanne Tan
OMG I thought I was just overworked lol. I was so tired for 3 weeks straight couldn't even lift my coffee cup. My doc said 'you're probably perimenopausal'... I went to a women's heart center on my own. Turns out I had microvascular disease. They saved my life. If you're tired and it's not normal? GO. NOW.
Annie Joyce
I work in cardiology and I can tell you the system is broken. We train on male data, test on male models, and dismiss women's symptoms as 'anxiety' until it's too late. I had a patient last month-38, active, no smoking, had SCAD after her baby. She was told she was 'just stressed.' She almost died. We need better protocols. And we need to stop calling women's symptoms 'atypical.' They're just different.
Rob Turner
I'm from the UK and I've seen this too. The NHS is starting to catch up, but it's slow. My sister-in-law had three ER visits before they tested for SCAD. She's 41. Healthy. No risk factors. Just... a woman. The data says it's rare. But it's happening. And we're not listening. We need to stop thinking of heart disease as a 'man's disease.' It's a human disease-with human differences.
Luke Trouten
It's not just about medical bias-it's about how we socialize women. We're taught to be polite, to not make a fuss, to 'tough it out.' So we wait. We downplay. We rationalize. And the system, built on male symptoms, doesn't see the urgency. We need to reframe this: if your body is screaming, you're not being dramatic. You're being smart. And doctors need to stop treating women's pain as a psychology problem.
Jason Pascoe
I'm a paramedic. We get called for 'just fatigue' or 'indigestion' all the time. I've seen too many women get sent home because their EKG looked 'fine.' But their troponin was rising slowly. We need to train crews to look beyond the textbook. And we need to trust women when they say 'something's off.'
Neha Motiwala
This is all a BIG PHARMA scam!!! They don't want you to know that heart disease is caused by 5G radiation and the government's fluoridated water!! They're selling you tests and drugs to keep you dependent!!! My cousin had a heart attack and she only ate kale and yoga!!
alex clo
The data presented here is compelling and aligns with recent clinical guidelines. It is imperative that healthcare providers prioritize gender-specific diagnostic pathways and that public health campaigns continue to emphasize the distinct presentation of cardiovascular events in women. Early intervention remains the cornerstone of improved outcomes.
Sonja Stoces
I'm sorry but this is just fearmongering. I'm 42, I eat avocado toast, I do yoga, and I'm fine. Why do we keep making women feel guilty for not being sick? Not every tired woman has microvascular disease. This article is making normal fatigue sound like a death sentence. 🤦♀️
Jonathan Noe
You all are missing the point. The real issue is that the American Heart Association only started funding women-specific research in 2023. That’s 75 years of neglect. We’ve been using male data since the 1940s. Of course we’re misdiagnosing. And now we’re scrambling? It’s not rocket science. Women’s bodies aren’t broken versions of men’s. They’re different. And we need to stop pretending otherwise.
Vamsi Krishna
I’ve been telling my sister for years she needs to get a coronary calcium scan. She’s 47, had gestational diabetes, and now she’s got 30% blockage. She didn’t believe it until she saw her own scan. I’m not a doctor but I googled enough to know: if you had preeclampsia, you’re not ‘fine.’ You’re a ticking time bomb. And no one told her. No one. That’s criminal.
Suzette Smith
I get it, but isn’t this just another way to make women feel like their bodies are broken? I mean, yes, heart disease is deadly. But now we’re telling women they need 17 different tests and to be paranoid about every yawn? I’m tired of being told I’m at risk just for being a woman.
Autumn Frankart
This is all part of the New World Order. They want us to think we’re fragile so we’ll take more pills, get more scans, and give up our autonomy. The real killer? Sugar. And Big Pharma. They don’t want you to know that a 10-minute walk and lemon water fixes everything. They want you scared. Stay woke.
Sophia Nelson
I read this whole thing. Honestly? Boring. I’ve had two heart attacks. No one told me anything. I just went to the ER. I got treated. I’m alive. Stop writing essays. Just tell women: if you feel weird, go to the hospital. That’s it.