Have you ever started a new medication and felt awful for the first few days-nausea, dizziness, fatigue-only to wake up one morning and realize those symptoms are gone? It’s not magic. It’s tolerance. And it’s happening in your body right now, at a cellular level, as your brain and organs adjust to the drug you’re taking.
Not all side effects disappear at the same rate. Some vanish within days. Others stick around for months-or never go away. That’s because tolerance isn’t one single process. It’s a mix of different biological changes, each affecting different parts of your body in different ways. Understanding this helps you know what to expect, when to worry, and when to talk to your doctor.
How Your Body Gets Used to Medications
Tolerance isn’t about your body ignoring the drug. It’s about your body changing how it responds. Think of it like turning down the volume on a speaker that’s too loud. Your nervous system, liver, and receptors all adapt to keep things balanced.
There are three main ways this happens. First, your liver gets faster at breaking down the drug. This is called pharmacokinetic tolerance. Some medications, like barbiturates or alcohol, trigger your liver to produce more enzymes-especially from the CYP450 family-that speed up metabolism. After a few weeks of regular use, your body clears the drug faster, so less of it sticks around to cause side effects.
The second way is pharmacodynamic tolerance. This happens at the receptor level. Imagine your brain has thousands of tiny locks (receptors) that the drug fits into. Over time, your body might shut down some of those locks, reduce how tightly the drug fits, or weaken the signal it sends after binding. For example, opioids bind to mu-opioid receptors. With repeated use, those receptors can decrease in number by 20-50%, making the drug less effective at triggering side effects like drowsiness or nausea.
The third mechanism is cellular adaptation. This is where things get even more specific. Your cells don’t just turn down the volume-they rewire themselves. Chronic alcohol use, for instance, changes the makeup of GABA-A and NMDA receptors in your brain. It increases certain protein subunits, like the NMDA R2B subunit, by 40-60%. This shifts your brain’s baseline, so it no longer reacts as strongly to the drug’s presence.
Why Some Side Effects Vanish-and Others Don’t
This is where it gets really practical. Not all side effects fade. Why? Because different systems in your body adapt at different speeds.
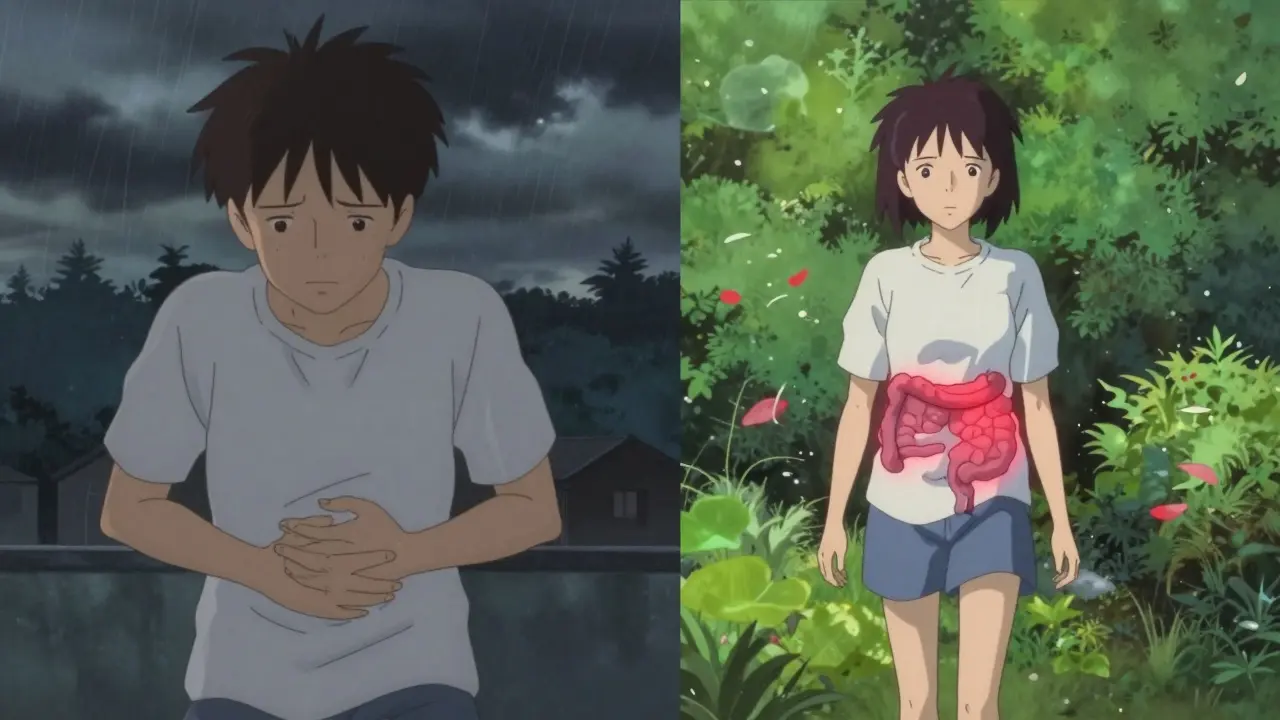
Take opioids. Most people taking them for pain notice nausea and dizziness fade within 3-7 days. But constipation? That rarely improves. Why? Because the receptors that cause constipation are mostly in the gut, and those cells don’t downregulate the same way brain receptors do. The gut doesn’t care about balance-it just keeps slowing down. That’s why doctors always prescribe laxatives alongside opioids from day one.
Benzodiazepines like Xanax or Valium follow a similar pattern. Sedation and drowsiness drop by 60-70% within two weeks. But the anxiety relief? That stays strong. Your brain adapts to the calming effect on sleep centers, but not on the fear circuits. That’s why these drugs can be used long-term for anxiety, even though you’re no longer sleepy after taking them.
Antidepressants like SSRIs (sertraline, fluoxetine) are another classic example. About 73% of people report nausea disappearing after 2-3 weeks. But sexual side effects-like trouble getting or keeping an erection-stick around for many. Why? Because serotonin receptors involved in sexual function don’t downregulate as easily as those in the stomach. Your brain tolerates the nausea, but not the sexual impact.
Even blood pressure meds like beta-blockers show this pattern. Fatigue and sluggishness often fade after 6-12 weeks. But the drop in blood pressure? That lasts. Your heart and blood vessels adjust to the drug’s effect on heart rate, but the overall pressure-lowering action remains steady.
Real Stories: What Patients Actually Experience
Real people report these patterns every day. On Reddit, over 78% of 1,245 users taking opioids for chronic pain said nausea disappeared in under a week-but constipation never did. One user wrote: “Started oxycodone after back surgery. Vomiting stopped after day 3. Constipation? Still on stool softeners six months later.”
On Drugs.com, 65% of people taking pregabalin for nerve pain said dizziness faded by day 14. By day 21, 82% had no dizziness left. But that doesn’t mean the drug stopped working. It just meant their brain adapted to the side effect, not the pain relief.
People on interferon beta-1a for multiple sclerosis report initial fatigue lifting after 4-6 weeks. But injection site reactions? Those stay. The immune system doesn’t learn to ignore the needle jab-it just learns to ignore the fatigue.
And then there’s the silent side effect: sexual dysfunction. A 2022 survey by NAMI found that while 73% of SSRI users got over nausea, 58% still struggled with sexual side effects after six months. That’s not rare. It’s expected.
What You Should Do When Side Effects Fade
When side effects disappear, it’s tempting to think the drug isn’t working anymore. It’s not. It just means your body adjusted. That’s actually a good sign-you’re tolerating the medication well.
But here’s the catch: don’t assume everything is fine just because you feel better. If your original symptoms (pain, anxiety, depression) are still there, the drug is likely still working. Don’t stop or lower your dose just because nausea is gone.
On the flip side, if a side effect that used to bother you is now gone, but a new one shows up-like weight gain, mood swings, or insomnia-that’s a signal. It could mean your body’s adapting in a new way. Talk to your doctor. You might need a dose tweak or a switch.
And never use tolerance as a reason to increase your dose on your own. That’s how dependence starts. If you feel like the medication isn’t helping anymore, it could be disease progression-not tolerance. Studies show 25-30% of patients and even some doctors mistake worsening symptoms for tolerance, when it’s actually the original condition getting worse.
When Tolerance Isn’t Tolerance
Tolerance is not addiction. It’s not dependence. It’s a biological adjustment. You can have tolerance without craving the drug. You can have tolerance without withdrawal symptoms.
But here’s the risk: if you start increasing your dose because you think “it’s not working anymore,” you’re feeding a cycle. Higher doses mean more receptor changes, more liver enzyme induction, and a greater chance of long-term side effects. It also makes quitting harder.
Some medications have built-in ways to fight tolerance. For example, nitroglycerin for heart pain causes tolerance if taken continuously. That’s why doctors recommend a “drug holiday”-a 10-12 hour break each day-so your body resets. Studies show this can restore effectiveness by 40-60%.
There’s also new research into “tolerance-resistant” formulations. One experimental version of oxycodone is wrapped in a polymer that releases the drug slowly, reducing how much the brain gets hit with sudden spikes. Early trials show 60% less tolerance development to respiratory depression after eight weeks.
What’s Next: Personalized Tolerance Predictions
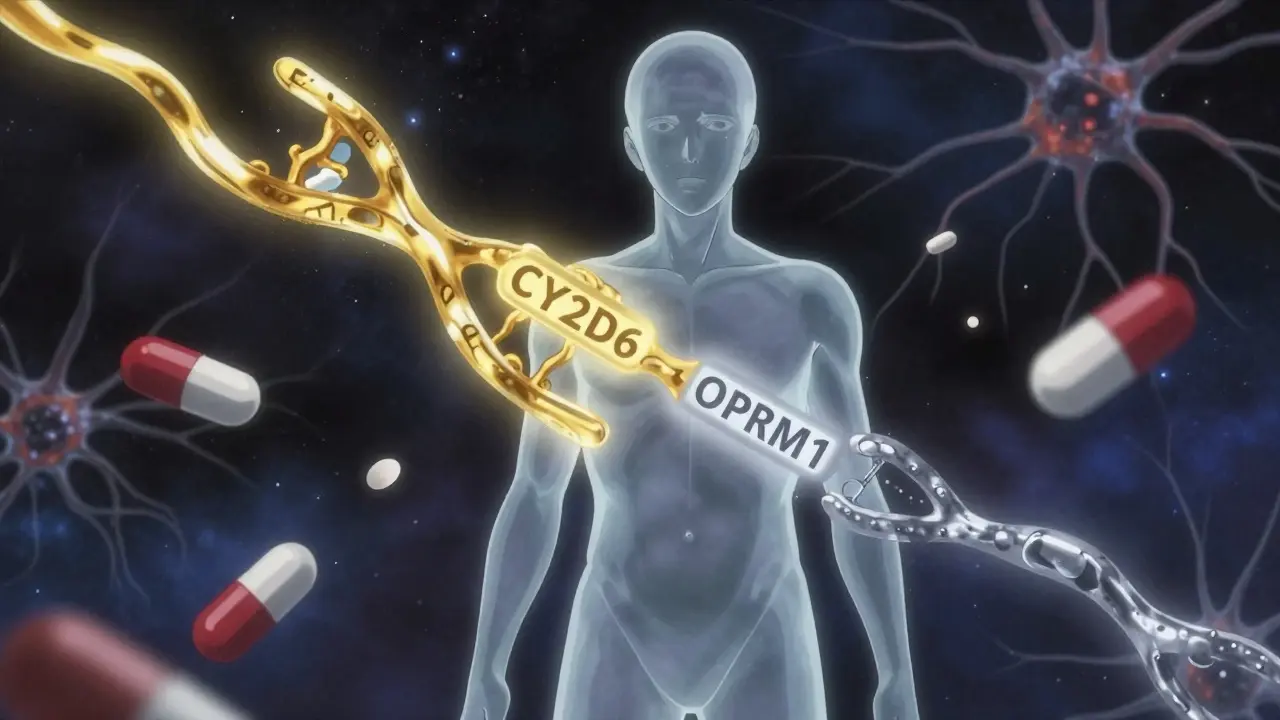
Science is getting better at predicting who will develop tolerance-and how fast. Genetic testing is starting to play a role. For example, 7-10% of Caucasians have a CYP2D6 gene variant that makes them poor metabolizers of codeine. That means they get little to no pain relief, not because the drug doesn’t work, but because their body can’t convert it to its active form.
Other genes, like OPRM1, affect how opioid receptors respond. Some people have a version that makes them naturally resistant to opioid side effects. Others have one that makes them develop tolerance rapidly. NIH has invested $127 million to map these differences and create genetic profiles that help doctors choose the right drug and dose from the start.
By 2030, most new brain and nervous system drugs will be designed with tolerance in mind. That means fewer side effects that stick around, and smarter ways to keep the good effects without the bad.
Bottom Line: Tolerance Is Normal-But Not Uniform
If you’re on a medication and side effects fade, don’t panic. It’s normal. Your body is doing exactly what it’s supposed to do: adapt. But don’t assume everything is fine just because you feel better. Some side effects vanish. Others don’t. And that’s okay-as long as you’re aware of it.
Keep track of what changes, when, and how it affects your daily life. Talk to your doctor if something new pops up, or if your original condition isn’t improving. Tolerance isn’t failure. It’s biology. And understanding it gives you more control over your treatment.

Katie Taylor
Finally someone explains why my SSRIs stopped making me puke but still wreck my sex life. No magic, just biology. I’ve been on sertraline for 14 months and still can’t orgasm, but at least I can eat breakfast without feeling like I’m gonna die. Your body’s not broken-it’s just doing its job. Don’t let anyone make you feel weird for needing meds that work, even if they come with baggage.
Side note: if your doctor acts surprised you still have sexual side effects after 6 months, fire them. This isn’t rocket science.
Sidra Khan
So let me get this straight-you’re telling me constipation from opioids doesn’t go away because your gut is too stubborn to adapt? Like, your colon just says ‘nope, I’m doing my thing’ while your brain’s like ‘oh cool, I’m chill now’? 🤦♀️
That’s the dumbest thing I’ve ever heard. Why didn’t evolution fix this? Why not just make the gut as smart as the brain? Someone’s been slacking.
Ademola Madehin
Y’all are acting like this is some deep scientific breakthrough. Bro, I’ve been on gabapentin for 8 years. Nausea? Gone in 3 days. Dizziness? Vanished by week 2. But the weight gain? The brain fog? The feeling like I’m walking through syrup while everyone else is sprinting? That’s my new normal.
And guess what? My doctor still acts like I’m exaggerating. Like I’m being dramatic. Like I’m not supposed to feel like a zombie just to stop my nerves from screaming. This isn’t tolerance-it’s a slow-motion betrayal by your own body.
And don’t even get me started on the ‘just talk to your doctor’ advice. You think they care? They’re just trying to get through their 12th patient of the day. I’m not a case study. I’m a person who’s tired.
suhani mathur
Let’s be real: if your doctor doesn’t warn you about the constipation with opioids before you start, they’re not doing their job. Same with sexual side effects on SSRIs. These aren’t ‘surprises’-they’re predictable, documented, and avoidable with proper counseling.
And yes, the gut doesn’t downregulate like the brain. That’s why we have laxatives. That’s why we have pelvic floor PT for SSRI-induced anorgasmia. That’s why you don’t just ‘wait it out’-you plan for it.
Stop acting like tolerance is some mystical force. It’s physiology. And physiology can be managed. You just need to ask the right questions before you start the med, not after you’ve been constipated for 3 months.
bharath vinay
They’re lying. All of this is corporate propaganda. The pharmaceutical companies don’t want you to know that tolerance isn’t biology-it’s designed. They engineer drugs to create dependence so you keep buying them. The ‘receptor downregulation’? That’s a cover story. The real reason side effects fade is because your body is starving for the drug. That’s not tolerance-that’s addiction. And they call it ‘adaptation’ to make you feel safe while they profit.
They know constipation doesn’t go away because they want you hooked. They know sexual dysfunction sticks because it keeps you ashamed and silent. This isn’t science. It’s a money machine.
And now they’re pushing ‘genetic testing’ so you’ll think it’s your fault you’re broken. Wake up.
Wilton Holliday
Just wanted to say thank you for writing this. I’ve been on beta-blockers for 2 years and thought I was just ‘getting old’ when the fatigue faded. Didn’t realize my body was adjusting. Now I know the blood pressure is still working-that’s huge.
Also, the bit about nitroglycerin breaks? That’s genius. I’ve never heard of that. My cardiologist never mentioned it. Maybe I’ll ask next time.
You’re right-tolerance isn’t failure. It’s adaptation. And knowing that makes me feel less like a broken patient and more like someone who’s learning how to work with their body. That’s powerful.
Joseph Manuel
While the article presents a superficially plausible narrative regarding pharmacokinetic and pharmacodynamic tolerance, it lacks critical nuance in its mechanistic claims. The assertion that opioid receptor downregulation occurs uniformly at 20–50% is an oversimplification derived from in vitro studies that do not reflect in vivo neuroadaptations in chronic pain populations. Moreover, the conflation of receptor density with functional efficacy ignores allosteric modulation and signaling bias, both of which are increasingly recognized as dominant factors in tolerance development. The cited Reddit and Drugs.com data are anecdotal and uncontrolled, rendering them statistically invalid for generalization. The suggestion that ‘tolerance is not addiction’ is technically correct but clinically misleading, as the neurobiological substrates of both overlap significantly in the mesolimbic dopamine pathway. This article risks reinforcing therapeutic nihilism among patients who may discontinue effective medications due to misinterpretation of adaptive physiology.
Harsh Khandelwal
So let me get this straight-you’re telling me my brain’s like a volume knob and my gut’s like a stubborn grandpa who won’t turn down the noise? 😂
Man, I’ve been on pregabalin for nerve pain and thought I was just getting used to the dizziness. Turns out my brain said ‘cool, I’m chill’ but my colon’s out here doing a slow-mo funeral march.
And don’t even get me started on the sex stuff. I thought I was just getting old. Nah. My serotonin receptors are just being petty. ‘You wanted mental peace? Fine. But you ain’t gettin’ no boner.’
Meanwhile, my doctor’s like ‘just wait, it’ll pass.’ Bro, I’ve been waiting since 2021. My wife’s side-eye is louder than my pain.
Andy Grace
This was really well put. I’ve been on an SSRI for anxiety for 18 months. The nausea vanished after two weeks. The insomnia? Took 3 months. The emotional numbness? Still there. I didn’t realize that was part of the same process.
It’s weird-when the side effects fade, you feel guilty for still feeling off. Like you’re being ungrateful. But this makes sense. My body adapted to the nausea, not the emotional side effects. That’s not weakness. That’s just biology being uneven.
Thanks for naming it. I feel less alone.
Spencer Garcia
Key takeaway: if a side effect fades, the drug is still working. If a new one shows up, talk to your doctor. If your original symptoms aren’t better, it’s not tolerance-it’s progression.
Don’t stop. Don’t increase. Just communicate.
Bret Freeman
They’re all lying. Tolerance isn’t biology-it’s a trap. They want you to think it’s normal that your body stops working right so you’ll keep taking the pills. Your liver doesn’t ‘adapt’-it’s being poisoned. Your receptors don’t ‘downregulate’-they’re being destroyed. And the ‘drug holiday’? That’s just a loophole so Big Pharma can say ‘see, we’re trying.’
Meanwhile, people are dying from withdrawal because they were told ‘it’s just tolerance.’ No. It’s addiction. And they’re hiding it behind fancy words.
Stop trusting doctors. Stop trusting science. Start asking: who profits?
Lindsey Kidd
Yessssss this is the kind of post I need when I’m Googling ‘why do I still feel like a zombie after 6 months on antidepressants’ 😭
Thank you for saying sexual side effects are common and not my fault. I thought I was broken. Turns out my brain just doesn’t care about my libido. 😅
Also-constipation with opioids? YES. I’m on oxycodone and still on Miralax. No shame. My colon is a stubborn beast. 🙌
Austin LeBlanc
So you’re telling me my body adapts to nausea but not to sexual dysfunction? That’s not biology. That’s patriarchy. Why does my brain care about vomiting but not about my sex life? Why is my pleasure less important than my stomach?
And why do doctors act like this is normal? Because they’re trained to ignore women’s pain. You think this is biology? It’s sexism with a lab coat.
And now they’re pushing genetic testing to make us think it’s our DNA’s fault? No. It’s the system’s fault. Fix the system, not the patient.
Katie Taylor
And yet, here I am-still on sertraline, still on laxatives, still not orgasming, but finally sleeping through the night and not crying in the shower every day. So yeah, tolerance sucks. But it also saved me. Don’t let anyone make you feel like you’re failing because your body learned to cope. You’re not broken. You’re surviving.
And if your doctor says ‘it’ll get better’ and doesn’t give you a plan? Find a new one. You deserve better than vague promises.