Ticlopidine Dosing Calculator for Kidney Function
Ticlopidine Dosing Calculator
Calculate appropriate ticlopidine dosing based on kidney function using the CKD-EPI equation.
Your Calculated eGFR
Key Monitoring Recommendations
For patients with eGFR < 60 mL/min, the following monitoring is recommended:
- Complete blood count (CBC) every 2 weeks for the first 3 months
- Monitor for neutropenia symptoms (fever, sore throat, mouth ulcers)
- Check platelet counts weekly for the first month
Ticlopidine Dosing Recommendations
Based on your kidney function, the appropriate ticlopidine dosing is:
| CKD Stage | eGFR (mL/min) | Recommended Dose | Risk Level |
|---|---|---|---|
| Stage 1 | ≥ 90 | 250 mg twice daily | Low |
| Stage 2 | 60-89 | 250 mg twice daily | Low |
| Stage 3 | 30-59 | 250 mg once daily | Medium |
| Stage 4 | 15-29 | 250 mg once daily | High |
| Stage 5 | < 15 | Not recommended | High |
Quick Takeaways
- Ticlopidine is cleared mainly by the liver, but its metabolites can affect the kidneys.
- Patients with chronic kidney disease (CKD) may need dose adjustments and closer monitoring.
- Compared with clopidogrel, ticlopidine has a higher risk of neutropenia and requires more lab checks.
- Monitoring glomerular filtration rate (GFR) and complete blood counts is essential when prescribing.
- Always discuss risks and benefits with your healthcare provider before starting or stopping the medication.
When it comes to blood‑thinners, ticlopidine often sits in the shadow of newer drugs like clopidogrel. Yet, many clinicians still encounter it, especially in patients who can’t tolerate alternatives. If you or someone you care for is prescribed ticlopidine, the big question is: how does it play with the kidneys? Below we break down the science, practical dosing tweaks, and the red‑flag labs you’ll want to watch.
What Is Ticlopidine?
Ticlopidine is a thienopyridine antiplatelet agent that inhibits platelet aggregation by irreversibly blocking the ADP‑P2Y12 receptor. It was first approved in the early 1990s for preventing stroke and reducing cardiovascular events after stent placement. Unlike aspirin, which works on multiple pathways, ticlopidine focuses on the ADP route, making it effective for patients who need a stronger blockade.
Because of its older‑generation status, ticlopidine carries a handful of safety concerns-most notably bone‑marrow suppression and gastrointestinal upset. These side effects have nudged many prescribers toward newer agents, but ticlopidine still has a niche, especially in patients with specific genetic profiles or drug‑interaction constraints.
How the Kidneys Handle Ticlopidine
Understanding renal handling starts with metabolism. After oral ingestion, ticlopidine is absorbed quickly (≈90% bioavailability) and undergoes extensive hepatic metabolism via the cytochrome P450 system, chiefly CYP2C19. The parent drug is cleared slowly (half‑life ~4-6hours), but its active metabolites linger longer-some are excreted unchanged in urine.
While the liver does most of the heavy lifting, the kidneys act as a final gate. In patients with normal renal function, about 20% of the dose is eliminated renally as metabolites. When kidney function drops, those metabolites can accumulate, raising the risk of off‑target effects such as neutropenia or platelet dysfunction.
Because the drug itself isn’t markedly nephrotoxic, the primary renal concern is indirect: impaired clearance leading to higher systemic exposure.
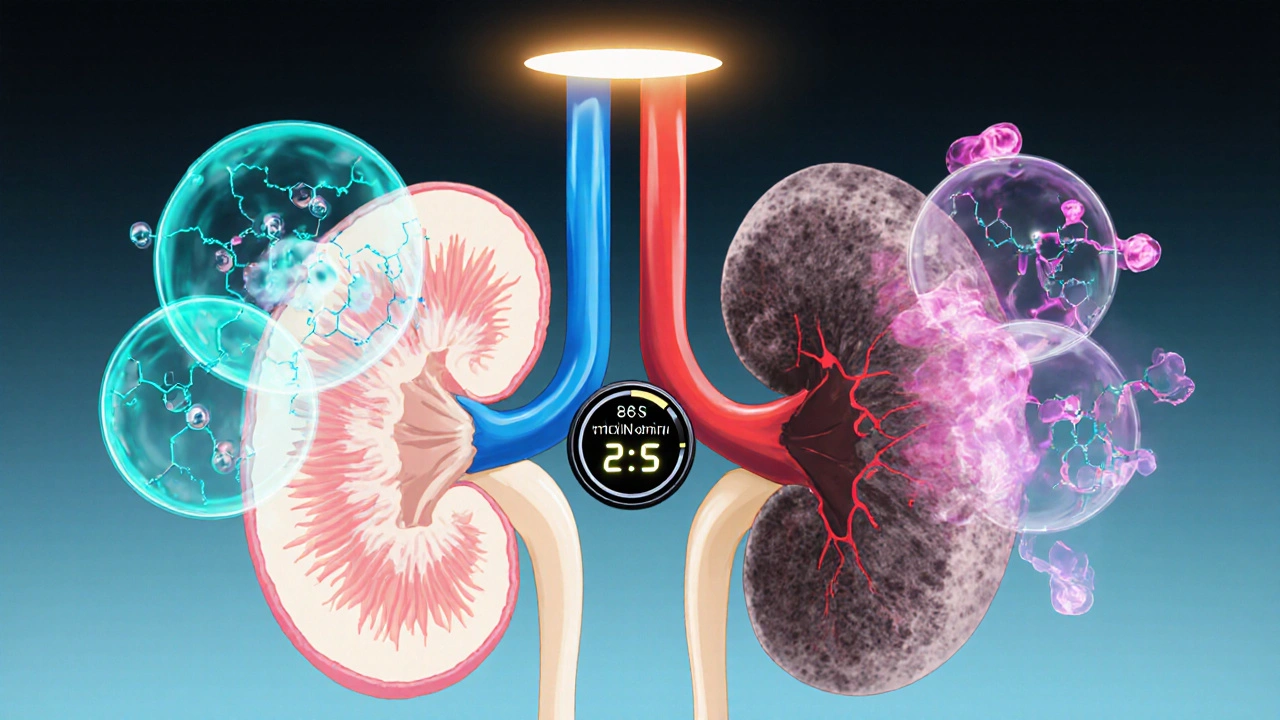
Renal Function and the Risk of Adverse Effects
Clinical data from the 1990s and early 2000s show a clear trend: patients with chronic kidney disease (CKD) experience a higher incidence of hematologic side effects. A 2003 observational study of 1,200 patients on ticlopidine reported a 12% neutropenia rate in those with an estimated glomerular filtration rate (eGFR)<30mL/min, versus just 3% in patients with eGFR>60mL/min.
Neutropenia, a dangerous drop in white blood cells, can predispose patients to infections. The mechanism isn’t fully understood but is thought to involve metabolite buildup that interferes with bone‑marrow progenitors. Additionally, platelet count drops (thrombocytopenia) have been noted, further compromising clotting balance.
These findings make routine blood‑count monitoring a must, especially in the first few weeks of therapy when the risk spikes.
Adjusting Ticlopidine Dosing in CKD
Unlike many antiplatelet agents, ticlopidine doesn’t have a universally accepted renal dosing algorithm. However, expert consensus and FDA guidance suggest the following pragmatic steps:
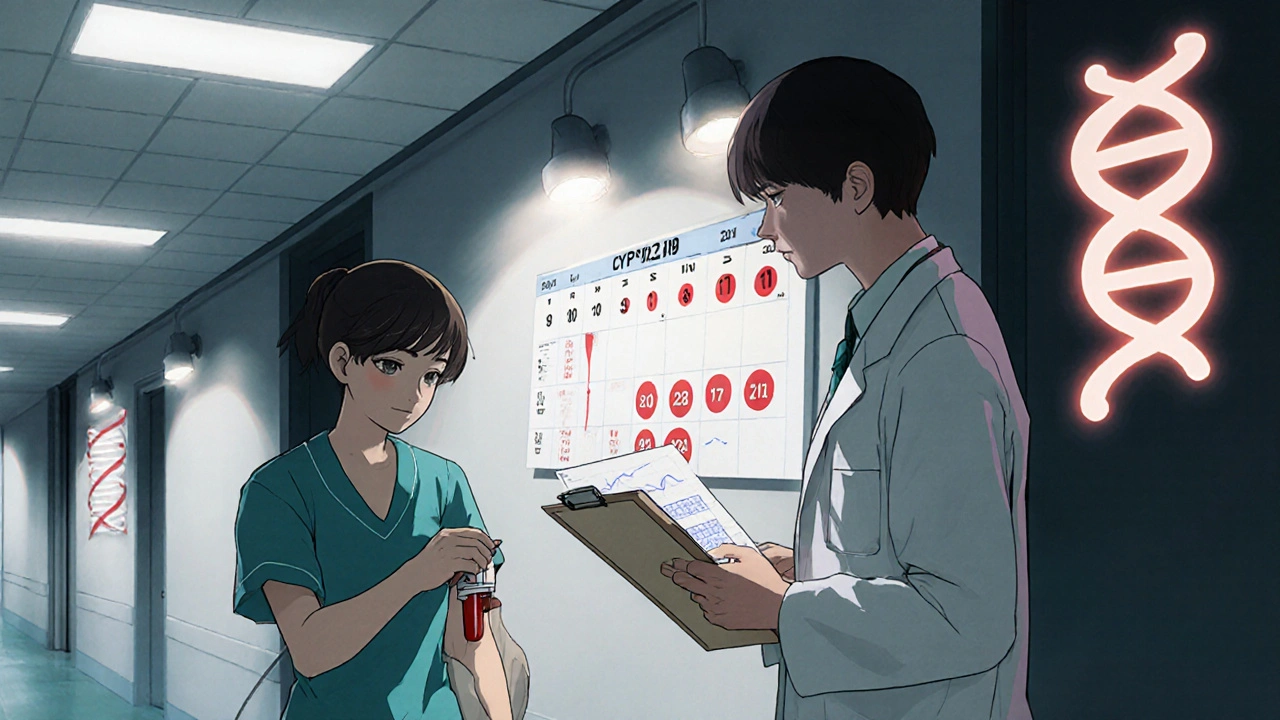
- Calculate eGFR using the CKD‑EPI equation for accuracy.
- If eGFR≥60mL/min, use the standard dose (250mg twice daily).
- For eGFR30‑59mL/min, consider reducing to 250mg once daily and increase monitoring frequency.
- If eGFR<30mL/min, many clinicians switch to clopidogrel or another antiplatelet, but if ticlopidine is essential, a dose of 125mg once daily with weekly CBCs for the first month is advised.
These adjustments aim to keep plasma concentrations within the therapeutic window while limiting metabolite pile‑up.
Comparing Ticlopidine and Clopidogrel: A Renal Perspective
Both drugs belong to the thienopyridine class, yet they differ in metabolism, renal handling, and safety profiles. Below is a side‑by‑side snapshot.
| Attribute | Ticlopidine | Clopidogrel |
|---|---|---|
| Primary metabolism | CYP2C19 (major) | CYP2C19 & CYP3A4 |
| Renal excretion (as metabolites) | ~20% | ~30% |
| Half‑life (active metabolite) | 7‑10hours | 6‑8hours |
| Standard dose | 250mg BID | 75mg BID |
| Risk of neutropenia | Higher (up to 12% in CKD) | Rare (<1%) |
| Typical monitoring | CBC weekly for 1month | Usually none |
| Contra‑indicated eGFR | eGFR<30mL/min (dose‑adjust) | None; use with caution |
Notice the higher neutropenia risk with ticlopidine, especially when kidneys aren’t filtering well. That’s why many clinicians prefer clopidogrel in CKD, but drug‑interaction profiles or genetic polymorphisms (e.g., CYP2C19 loss‑of‑function) can tilt the decision back toward ticlopidine.
Monitoring Strategies: Labs and Clinical Signs
Effective monitoring blends lab work with symptom awareness. Here’s a concise checklist:
- Baseline CBC before starting therapy.
- Repeat CBC at week1, week2, and week4; then monthly for the first 3months.
- Track eGFR every 3months, or sooner if the patient has fluctuating kidney function.
- Watch for fever, sore throat, or unusual bruising-early signs of neutropenia or thrombocytopenia.
- Educate patients to report any new infections or bleeding promptly.
If neutrophil counts drop below 1,000cells/µL, pause ticlopidine and consider switching agents. For platelet counts <100,000/µL, dose reduction or discontinuation is recommended.
Practical Tips for Patients and Clinicians
Bridging the science to daily practice, keep these nuggets in mind:
- Medication reconciliation: Ensure patients aren’t taking other drugs that inhibit CYP2C19 (e.g., omeprazole), which can raise ticlopidine levels.
- Use eGFR calculators built into EMR systems to avoid manual errors.
- Set up automatic lab reminders-most EMRs allow ordering repeat CBCs with one click.
- Consider genetics: patients who are CYP2C19 poor metabolizers may experience higher active metabolite exposure, increasing risk.
- When switching from ticlopidine to clopidogrel (or vice‑versa), allow a 48‑hour washout to reduce overlapping antiplatelet effect.
Open communication is key. Many patients fear “blood thinners” but don’t realize the difference in monitoring needs. A quick conversation about the purpose of weekly blood draws can improve adherence.
Frequently Asked Questions
Can I take ticlopidine if I have stage 3 CKD?
Yes, but the dose is usually reduced to 250mg once daily, and you’ll need close monitoring of CBC and eGFR for the first month.
Why is neutropenia more common with ticlopidine than clopidogrel?
Ticlopidine’s metabolites, which accumulate when kidneys are sluggish, can directly suppress bone‑marrow production. Clopidogrel’s metabolites are less toxic, so neutropenia is rare.
Do I need to stop ticlopidine before surgery?
Typically, stop ticlopidine 7days prior to most surgeries to allow platelet function to recover. Discuss timing with your surgeon and cardiologist.
Is there a simple test to know if I’m a CYP2C19 poor metabolizer?
Genetic testing labs offer a CYP2C19 panel. Results guide whether ticlopidine dosing needs adjustment or if an alternative agent is safer.
Can I switch from ticlopidine to clopidogrel without a washout period?
A short 48‑hour washout is recommended to avoid overlapping antiplatelet effects, which could raise bleeding risk.
Steve Holmes
Hey folks!!!, just wanted to add that while ticlopidine isn’t primarily renally cleared, you still gotta watch those metabolite levels, especially if eGFR dips below 60, because the kidneys become the final checkpoint!!!, also remember to schedule CBCs at baseline, then at week 2 and week 4, because neutropenia can sneak in fast!!!, and if you’re on other CYP2C19 inhibitors, dose‑adjustments might be warranted!!!, stay safe!!!
Tom Green
That’s a solid summary, Steve. I’d add that calculating eGFR with the CKD‑EPI equation gives a more accurate picture than the older MDRD, which helps when deciding whether to halve the dose. Also, keeping an eye on the patient’s medication list for CYP2C19 substrates can prevent hidden interactions.
Emily Rankin
Imagine the journey of a single molecule of ticlopidine, soaring through the bloodstream, only to meet the vigilant gates of the kidneys. In patients with robust renal function, it passes unscathed, but when the filters falter, each metabolite becomes a lingering echo of risk. Yet, hope shines through: diligent monitoring transforms potential peril into proactive care, empowering patients to stay within the rhythm of health.
Rebecca Mitchell
Kidney issues change drug clearance and blood counts need checking often
Roberta Makaravage
Ticlopidine, though older, still finds a niche in modern therapy. Its hepatic metabolism via CYP2C19 produces metabolites that are partially excreted by the kidneys. When eGFR falls below 60 mL/min, these metabolites accumulate, raising the specter of hematologic toxicity. Neutropenia, a dreaded side effect, has been documented in up to 12 % of patients with chronic kidney disease. This is why baseline complete blood counts are non‑negotiable before initiation. Moreover, repeat CBCs at weeks two, four, and then monthly for the first three months are essential. If a patient’s platelet count drops below 150 × 10⁹/L, clinicians must reconsider the regimen immediately. Dose adjustment is not set in stone, but many experts recommend halving the dose for eGFR 30‑59 mL/min. For eGFR below 30 mL/min, some even advocate switching to clopidogrel or another agent due to safety concerns. Drug‑drug interactions further complicate the picture; proton‑pump inhibitors can inhibit CYP2C19, enhancing ticlopidine levels. Patients on omeprazole, therefore, should be monitored even more closely. The literature also hints at a possible link between metabolite buildup and platelet dysfunction, though more research is needed. In practice, the mantra should be “monitor, monitor, monitor” – a simple yet powerful directive. Education of patients is crucial; they must understand why frequent lab draws are required. Empowered patients are more likely to adhere to monitoring schedules, reducing the risk of adverse events. Bottom line: ticlopidine can be safe in CKD when we respect the pharmacokinetic realities – and a few emojis don’t hurt 😊🚀💊.
Lauren Sproule
Totally get what you’re saying Roberta the “monitor monitor monitor” vibe is spot on I think it helps if we keep it simple for patients 😅
CHIRAG AGARWAL
Sounds like a lot of hassle for a drug nobody uses.
genevieve gaudet
From a holistic view, the body’s clearance pathways are like cultural bridges – when one side falters, the other must adapt, reminding us that medicine is as much an art as a science.
Patricia Echegaray
But what they don’t tell you is that big pharma sneaks these “old‑school” meds into our charts to keep us dependent, a subtle empire of control masked as “clinical choice”.
Miriam Rahel
While the author provides a cursory overview, a rigorous appraisal of the pharmacokinetic data reveals several omissions, notably the absence of a stratified dosing algorithm based on precise eGFR thresholds, which undermines the utility of the guide for seasoned clinicians.
Samantha Oldrid
Oh, brilliant – because we all have time to read dense textbooks during rounds.
Malia Rivera
Ultimately, the interplay between hepatic metabolism and renal excretion reflects a deeper truth: every therapeutic decision is a negotiation between the body’s intrinsic rhythms and our engineered interventions.