Levothyroxine is one of the most commonly prescribed drugs in the U.S., with over 127 million prescriptions filled in 2022 alone. It’s the go-to treatment for hypothyroidism - a condition where the thyroid doesn’t make enough hormone. For many, it’s life-changing: fatigue fades, weight stabilizes, brain fog lifts. But here’s the catch: levothyroxine isn’t a set-it-and-forget-it pill. Get the dose wrong, switch brands without telling your doctor, or skip blood tests, and you could end up with symptoms that feel worse than the original condition.
Why Levothyroxine Works - and Why It Can Go Wrong
Levothyroxine is a synthetic version of T4, the main hormone your thyroid makes. Your body converts T4 into T3, the active form that powers your metabolism, heart, brain, and muscles. When your thyroid fails, levothyroxine steps in. But because thyroid hormones affect nearly every cell in your body, even tiny changes in dosage matter. Too little, and you stay tired, cold, and gaining weight. Too much, and you get heart palpitations, anxiety, bone loss, or even atrial fibrillation.
The problem isn’t the drug itself. It’s how it’s managed. Studies show 90% of patients feel better within 3 to 6 months - but only if their dose is right. That’s where monitoring comes in. Without regular blood tests, you’re guessing.
How Often Should You Get Tested?
When you first start levothyroxine, your doctor should check your TSH (thyroid-stimulating hormone) level after 6 weeks. That’s not a suggestion - it’s a requirement. TSH tells you how hard your pituitary gland is working to stimulate your thyroid. If it’s high, you’re under-treated. If it’s low, you’re over-treated.
After the first test, follow-ups happen every 3 months until your levels are stable. Once you’re steady - meaning two TSH readings in range, 3 months apart - you can drop to once a year. But here’s where things break down: only 58% of U.S. primary care practices follow this schedule. Over a third of patients go 18 months or longer without a test, even when they’re still having symptoms.
There are exceptions. If you’re pregnant, your dose needs checking every 4 to 6 weeks. If you’re over 65 or have heart disease, adjustments happen slower - usually 25 mcg at a time. If you’ve had thyroid cancer, your target TSH might be kept very low, sometimes below 0.1. One size does not fit all.
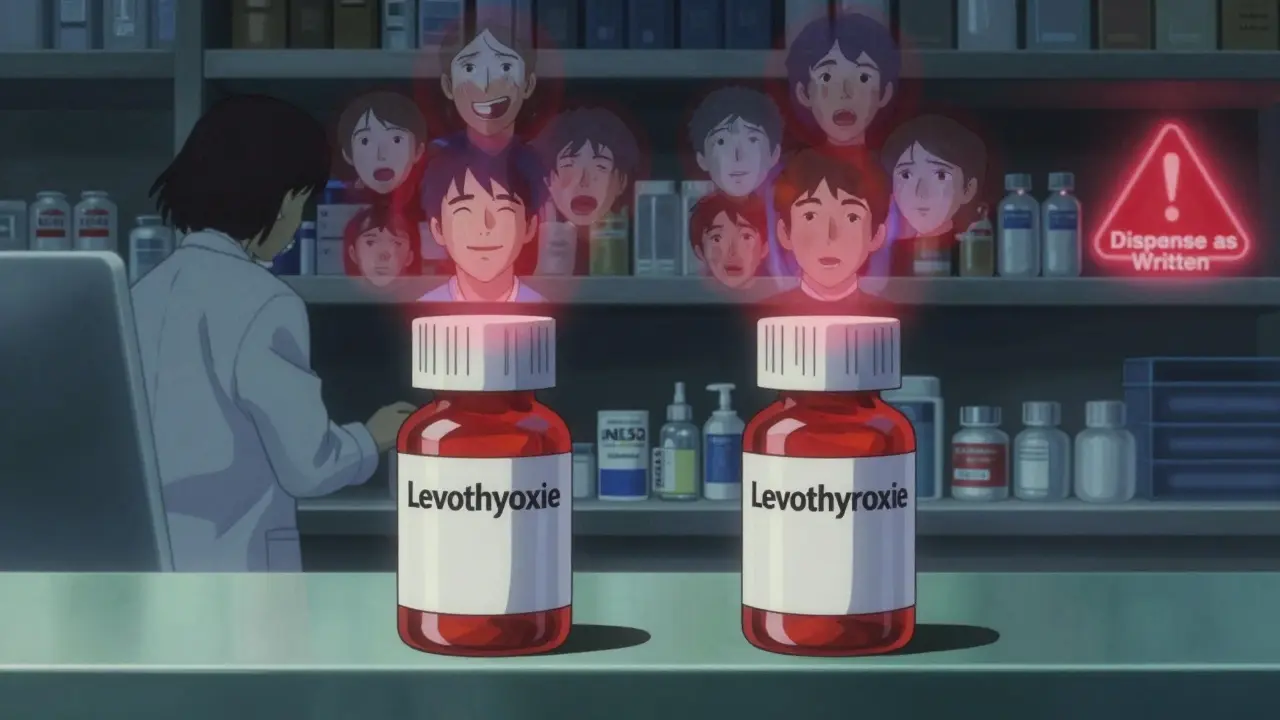
Brand Switching Is a Hidden Risk
You might think all levothyroxine is the same. After all, they’re all labeled 50 mcg, 75 mcg, 100 mcg. But different manufacturers use different fillers and binders. For most people, that doesn’t matter. For some, it does.
The UK’s Medicines and Healthcare products Regulatory Agency (MHRA) collected 335 reports of problems after patients switched brands between 2015 and 2019. Symptoms? Fatigue (78%), headaches (65%), anxiety (47%), and heart palpitations (39%). Only 27 of those cases had thyroid blood tests done - meaning most doctors didn’t know if the patient was under- or over-medicated.
Patients on forums like Thyroid UK and Reddit’s r/Hashimotos report that 68% of them had symptoms return after a pharmacy substitution. One woman in Seattle switched from a brand-name version to a generic and started having panic attacks. Her TSH jumped from 2.1 to 6.8 - she was suddenly under-treated. She had to go back to the original brand to feel normal again.
Doctors now advise: if you’ve ever had trouble after a switch, ask your prescriber to write "Dispense as written" or specify the brand name on your prescription. Pharmacists can still switch it unless the doctor blocks it.
What You Need to Know About Taking It Right
Levothyroxine doesn’t work well if you take it with food, coffee, or supplements. It’s absorbed best on an empty stomach, 30 to 60 minutes before breakfast. Taking it with calcium, iron, antacids, or even soy milk can cut absorption by half.
If you take a calcium supplement at breakfast, wait at least 4 hours before taking your thyroid pill. Same with iron pills, multivitamins, or cholesterol meds like cholestyramine. Even coffee - especially if it’s strong - can interfere. Some people take it at bedtime instead, which works just as well as long as it’s still on an empty stomach and at least 3 hours after your last meal.
Who Needs Extra Care?
Not everyone can be treated the same. You need specialist input if you’re:
- Under 16
- Pregnant or in the first year after giving birth
- Have heart disease, especially atrial fibrillation or angina
- Have adrenal insufficiency (Addison’s disease)
- Take lithium or amiodarone (used for heart rhythm issues)
- Have pituitary or hypothalamic disease
These groups are at higher risk of complications. Dose changes need to be slower. Monitoring needs to be tighter. Skipping a test isn’t an option.

The Bigger Picture: Why Monitoring Falls Through the Cracks
Levothyroxine is cheap, generic, and widely available. That’s great for access - but it also makes it easy to treat like a routine refill. Primary care doctors, juggling dozens of patients, may not realize how sensitive thyroid levels are. Nurses might not flag abnormal TSH results. Pharmacies don’t notify doctors when substitutions happen.
Patients, too, often don’t speak up. They assume fatigue and weight gain are just part of aging. Or they think, "My doctor didn’t call, so everything must be fine." But thyroid dysfunction creeps up slowly. By the time symptoms are obvious, your body’s been out of balance for months.
Studies show that 15% to 20% of patients need a dose change every year - due to aging, weight gain, new medications, or even seasonal changes. Your needs aren’t static. Your treatment shouldn’t be either.
What You Can Do Right Now
If you’re on levothyroxine, here’s what to do:
- Know your last TSH number. Write it down.
- Check when your last blood test was. If it’s been over a year, schedule one.
- Ask your pharmacist: "Is this the same brand I’ve been taking?" If it changed, tell your doctor.
- Take your pill on an empty stomach, 30 minutes before food or coffee.
- Keep a list of all your supplements and meds. Bring it to every appointment.
- If you feel worse - even slightly - don’t wait. Get tested.
There’s no magic formula. But if you stay informed and stay proactive, you can avoid the pitfalls most people don’t even know exist.
Is There a Better Alternative?
Some patients still feel off even with normal TSH levels. For them, combination therapy - adding liothyronine (T3) to levothyroxine - is being studied. But the American Thyroid Association doesn’t recommend it as standard. Most guidelines say: fix the T4 dose first. Only consider T3 if you’ve done everything right and still have symptoms.
Right now, levothyroxine remains the gold standard. It’s safe, effective, and affordable - when used correctly. The real issue isn’t the drug. It’s the system around it.
How long does it take for levothyroxine to start working?
You may notice small improvements in energy or mood within 2 to 3 weeks, but it takes 4 to 6 weeks for your body to fully adjust to a new dose. Full symptom relief usually happens within 3 to 6 months after your dose is stabilized. Don’t rush dose changes - give your body time to respond.
Can I stop taking levothyroxine if I feel better?
No. Hypothyroidism is usually a lifelong condition. Stopping the medication will cause your symptoms to return - often worse than before. Even if you feel fine, your thyroid isn’t producing hormones on its own. Levothyroxine isn’t a cure; it’s a replacement. Stopping it can lead to dangerous complications like myxedema coma in extreme cases.
Why do some people still feel tired even with normal TSH?
Normal TSH doesn’t always mean optimal thyroid function. Some people have trouble converting T4 to T3, the active hormone. Others have autoimmune inflammation that persists even with hormone replacement. In rare cases, nutrient deficiencies (like low iron or vitamin D) can mimic hypothyroid symptoms. If you’re still tired, ask your doctor to check Free T3, reverse T3, ferritin, and vitamin D - not just TSH.
Is it safe to take levothyroxine long-term?
Yes - when monitored properly. Millions of people take levothyroxine for decades without issues. The risks come from incorrect dosing, not the medication itself. Too much can weaken bones or trigger heart problems, especially in older adults. Too little leaves you at risk for high cholesterol, heart disease, and depression. Regular blood tests are the only way to stay safe.
What should I do if my pharmacy changes my brand?
If you notice new symptoms after a brand switch - fatigue, anxiety, heart racing, weight changes - contact your doctor right away. Request a TSH test. Ask your prescriber to write "Dispense as written" or specify the brand name on future prescriptions. You have the right to request the same formulation you’ve been on. Don’t assume it’s "the same dose" - it might not be the same for your body.

Solomon Ahonsi
Wow, another one of those "just take your pill and shut up" medical guides. Meanwhile, my TSH jumped from 2.5 to 8.3 after my pharmacy switched me to a generic without telling me. My doctor didn’t even blink. Thanks for the 127 million prescriptions stat - tells me how many people are just surviving, not living.
George Firican
It’s fascinating how we’ve turned a physiological balancing act into a bureaucratic checkbox. Levothyroxine isn’t a drug - it’s a mirror reflecting the fragmentation of our healthcare system. We prescribe it like it’s aspirin, yet it regulates the very engine of metabolism, cognition, and emotional resilience. And we wonder why people feel off. The system doesn’t see the person - only the lab value. TSH is a proxy, not a prophet. Real healing requires listening, not just testing.
Matt W
Been on levothyroxine for 8 years. Switched brands last year - started having panic attacks at 3am. Got my TSH checked - up to 7.2. Went back to my original brand and felt human again. Why is this still not standard practice? Pharmacies shouldn’t be playing Russian roulette with people’s hormones.
Anthony Massirman
Take it on an empty stomach. No coffee. No calcium. Period. If you can’t do that, don’t complain when you’re still tired.
jay patel
bro i took mine with my morning chai and now i feel like a zombie on a treadmill. my doc said "tsh is fine" but my brain is still stuck in 2019. also my pharmacy switched me to some indian generic and now my hands shake. i think my body is mad at me. or maybe the pharmacy. idk anymore.
Hannah Gliane
Of course you feel bad - you probably take it with your oat milk latte and then chug a calcium supplement like it’s a protein shake. You think your body is a magic box that ignores chemistry? 🤦♀️ Get your act together. TSH isn’t a suggestion. It’s your body screaming.
Ellie Norris
I’m a nurse in the UK and I’ve seen this so many times. Patients come in saying they’re exhausted, but their last test was 18 months ago. We always check TSH, FT3, FT4, ferritin, vit D - but GPs often don’t. And when they do, they only look at TSH. It’s heartbreaking. If you’re still tired, ask for the full panel. You deserve to feel better.
Chinmoy Kumar
so i read this whole thing and i still dont get why my doc wont let me try t3. i feel fine on t4 but my energy is just... flat. like i'm running on 20% battery. everyone says "just wait" but what if waiting is the problem? also i think my thyroid is haunted. just saying.
Gary Mitts
My TSH was 0.1 last year. I was sweating through my shirts. Doctor said "you’re fine". I went to a new doc. They changed my dose. I cried. I actually cried. Because for the first time in years, I didn’t feel like I was going to die from anxiety. Don’t trust the system. Trust your body.
clarissa sulio
U.S. doctors are the best. If you’re having issues, you’re probably doing it wrong. Take your pill. Stop complaining. We’ve got real problems here - like border security and inflation. Your thyroid isn’t a political issue.
Bridget Molokomme
so i switched to bedtime dosing and it changed my life. no more coffee conflicts, no more forgetting. i just take it after brushing my teeth and go to sleep. my tsh is perfect. why is this not common knowledge? also, i’m now obsessed with thyroid health. my cat’s on a thyroid diet now. i’m not kidding.
Vatsal Srivastava
Levothyroxine? Please. It’s just a placebo for people who don’t understand stress. I’ve been on it for 5 years. My TSH is normal. I still feel awful. Turns out the real problem is capitalism. Also, your doctor is probably just lazy. And yes, I know more than your endocrinologist.