When you hear the word obesity, most people think of weight alone. But for millions of people, obesity isn’t just about fitting into clothes or climbing stairs. It’s the root of a dangerous trio: type 2 diabetes, heart disease, and sleep apnea. These three conditions don’t just happen at the same time-they feed each other, making every one worse. And if you’re living with obesity, ignoring one means you’re putting yourself at higher risk for the others.
How Obesity Triggers Diabetes
Obesity doesn’t just add extra pounds-it changes how your body works. Fat tissue, especially around the belly, releases chemicals that cause chronic low-grade inflammation. This inflammation messes with insulin, the hormone that tells your cells to take in sugar from your blood. When insulin stops working right, your blood sugar rises. That’s type 2 diabetes.
People with obesity are 3 to 5 times more likely to develop diabetes than those at a healthy weight. But it’s not just about how much you weigh. Where the fat is stored matters too. A waist size over 40 inches in men or 35 inches in women increases diabetes risk even if your BMI is only slightly above normal. That’s because abdominal fat is more active in triggering insulin resistance.
And here’s the catch: once diabetes sets in, it makes weight loss harder. High blood sugar leads to more hunger and fatigue, which can make sticking to a diet or exercise plan feel impossible. It’s a cycle: obesity causes diabetes, and diabetes makes obesity harder to treat.
Why Sleep Apnea Is More Than Just Snoring
If you snore loudly, wake up gasping, or feel exhausted even after a full night’s sleep, you might have obstructive sleep apnea (OSA). It’s not just annoying-it’s deadly when you’re overweight.
Extra fat around your neck and tongue narrows your airway. When you lie down, that airway collapses, stopping your breathing for 10 seconds or more, sometimes hundreds of times a night. Your brain wakes you up just enough to breathe again-without you even realizing it. That’s why you’re tired all day, even if you think you slept well.
Studies show that 86% of obese people with type 2 diabetes also have OSA. And it’s not just about weight: each extra point on your BMI increases your risk of sleep apnea by 14%. Waist size is an even stronger predictor than BMI. For every centimeter your waist grows, your chance of sleep apnea goes up by 12%.
But here’s what most doctors don’t tell you: sleep apnea makes diabetes worse. When your breathing stops, your oxygen levels drop. That triggers stress hormones, which spike your blood sugar. One study found that people with severe sleep apnea had 30% more insulin resistance than those without it-even when they weighed the same.
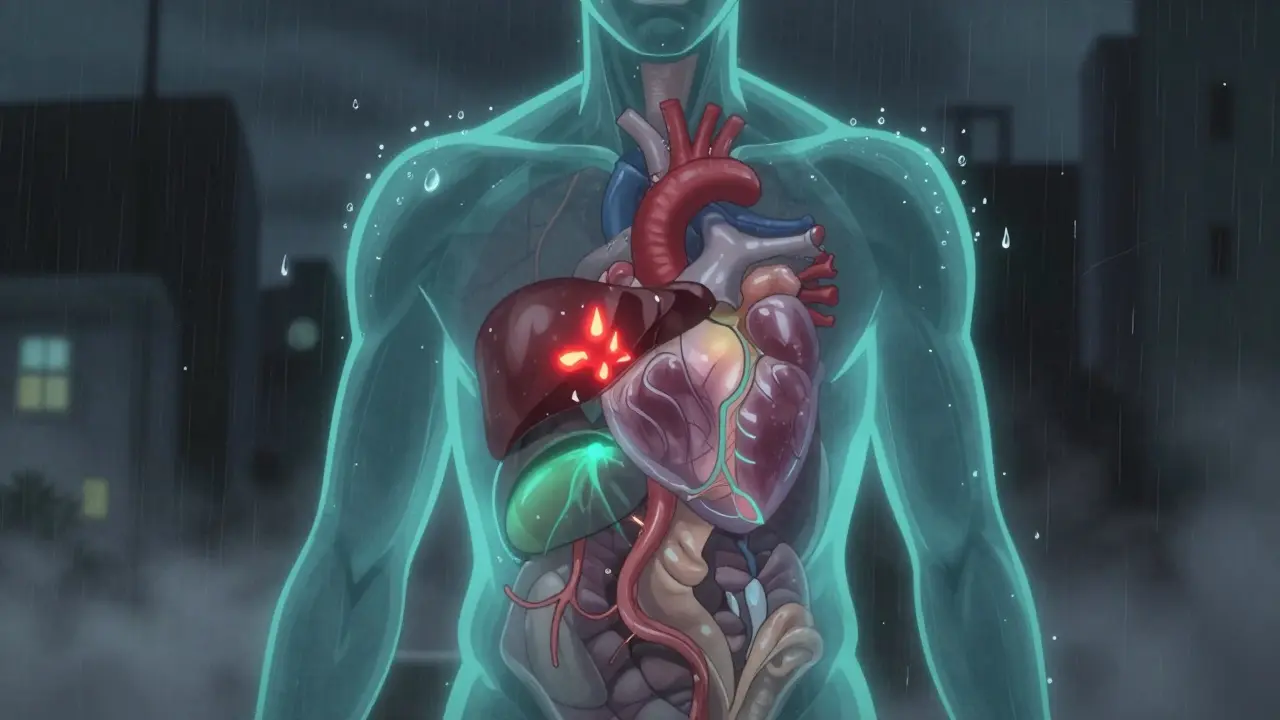
The Hidden Link to Heart Disease
Now put it all together. Obesity causes insulin resistance. Insulin resistance leads to high blood sugar. High blood sugar damages blood vessels. Sleep apnea causes your blood pressure to spike every time you stop breathing. That’s 20-30 mmHg spikes, night after night. Your heart has to work harder, and your arteries start to harden.
People with obesity, diabetes, and sleep apnea have a 3.2 times higher risk of heart attack than someone with none of these conditions. The combination doesn’t just add risk-it multiplies it. One study found that obese people with sleep apnea are 2.3 times more likely to develop heart failure than those with obesity alone. Add diabetes, and that risk jumps to 3.7 times higher.
And it’s not just heart attacks. Sleep apnea increases stroke risk by 68% and raises the chance of atrial fibrillation (an irregular heartbeat) by 2 to 5 times in severe cases. In fact, sleep apnea is responsible for about 6.4% of the heart rhythm problems linked to obesity. That means even if you control your weight, untreated sleep apnea is still quietly damaging your heart.

Why Most People Miss the Connection
Here’s the problem: doctors often treat each condition in isolation. A diabetic patient gets blood sugar meds. Someone with sleep apnea gets a CPAP machine. A person with high blood pressure gets a beta-blocker. But rarely do they look at the whole picture.
Patients report waiting 5 to 7 years to get diagnosed with sleep apnea-even when they’re clearly obese and diabetic. Why? Because many doctors don’t screen for it. The American Diabetes Association says all obese diabetics should be checked for sleep apnea. But only 18% of them actually are.
And even when diagnosed, treatment fails. Only 45% of people keep using their CPAP machine after a year. Why? Masks are uncomfortable. Some feel claustrophobic. Others can’t stand the air pressure. It’s not laziness-it’s a system that doesn’t support long-term adherence.
What Actually Works: Breaking the Cycle
The good news? You don’t have to live with all three. Each one can be reversed-even if you’ve had them for years.
Weight loss is the most powerful tool. Losing just 10% of your body weight reduces sleep apnea severity by half. It lowers blood sugar, improves insulin sensitivity, and reduces pressure on your airway. One study showed that obese diabetics who lost 10% of their weight dropped their HbA1c (a measure of long-term blood sugar) by 0.8%-enough to reduce medication needs.
CPAP works-but only if you use it. Using CPAP for at least 4 hours a night reduces heart attacks and strokes by 28% in people with obesity and diabetes. It also improves blood sugar control. But you need support. Talk to your doctor about trying different masks, adjusting pressure settings, or using a humidifier. Some people do better with oral appliances or newer treatments like hypoglossal nerve stimulation, which keeps your airway open without a mask.
Medications can help too. New diabetes drugs like semaglutide (Wegovy, Ozempic) don’t just lower blood sugar-they cause significant weight loss. In one trial, patients lost nearly 15% of their body weight, and their sleep apnea improved even before the full weight loss happened. That’s because these drugs reduce fat around the neck and throat, not just overall weight.
Surgery is an option for some. Bariatric surgery leads to remission of sleep apnea in 78% of cases and diabetes in up to 80%. But it’s not for everyone. The risks are real, and you need lifelong follow-up.
How to Get Started Today
You don’t need to fix everything at once. Start here:
- Get screened. If you’re obese and have diabetes, ask your doctor for a sleep apnea screening. The STOP-Bang questionnaire takes less than a minute. If your score is 3 or higher, you need a sleep study.
- Track your waist. Measure your waist every month. If it’s over 40 inches (men) or 35 inches (women), focus on reducing belly fat.
- Move more. Even 30 minutes of walking a day improves insulin sensitivity and reduces sleep apnea events.
- Ask about GLP-1 medications. If you’re struggling to lose weight, talk to your endocrinologist. These drugs are changing the game.
- Don’t give up on CPAP. If you quit, go back. Try a different mask. Ask for a pressure adjustment. Use a humidifier. It’s worth it.
What’s Next: The Future of Treatment
Doctors are starting to treat these three conditions as one problem-not three separate ones. New programs in places like Kaiser Permanente are linking endocrinologists, sleep specialists, and cardiologists into the same care team. They track weight, blood sugar, and sleep apnea severity together. So far, hospital visits have dropped by 22%.
Technology is helping too. New smartphone apps can now predict sleep apnea severity by analyzing your breathing patterns and blood sugar levels overnight. In 2024, a study showed these tools could detect sleep apnea with 85% accuracy-no sleep lab needed.
But the biggest challenge isn’t medical. It’s systemic. We still treat obesity like a personal failure, not a complex disease. And until we change that, we’ll keep missing the chance to stop this deadly triad before it takes your heart, your sleep, or your life.
Real Change Starts With Awareness
Obesity isn’t the enemy. The real enemy is ignoring how it connects to everything else. You can’t manage diabetes without checking for sleep apnea. You can’t protect your heart without treating both. And you can’t break the cycle by focusing on one thing alone.
It’s time to stop treating symptoms and start treating the root. If you have obesity and one of these conditions, ask: Could I have the others? Get tested. Talk to your doctor. Don’t wait until it’s too late.
Alec Amiri
Look, I’ve seen this a hundred times-fat guy gets diabetes, gets CPAP, still eats pizza at 2 a.m. and wonders why he’s dying. It’s not rocket science. Lose weight. Move. Stop blaming the system. Your couch isn’t your therapist.
Lana Kabulova
Okay-but have you ever tried using a CPAP machine when you’re claustrophobic, your nose is dry, and your partner keeps stealing the blanket? It’s not that people don’t want to comply-it’s that the system gives you a $3,000 mask and says ‘good luck’? No support. No follow-up. No empathy. Just a beep and a bill.
Mike P
Y’all are overcomplicating this. In America, we used to just tell people to eat less and move more. Now we’ve got GLP-1 drugs, sleep labs, and endocrinologists playing detective like it’s a Netflix doc. Meanwhile, in India, my cousin lost 80 lbs walking 5 miles a day to the market-no machines, no meds, just willpower. Stop medicalizing laziness.
Keith Helm
It is imperative to recognize that the interplay between metabolic dysfunction, respiratory compromise, and cardiovascular strain constitutes a triad of pathophysiological synergy, which, if left unaddressed in a coordinated clinical framework, inevitably exacerbates morbidity and mortality. Systemic intervention is not optional-it is a medical imperative.
Akriti Jain
Big Pharma paid these doctors to make you think you need a $1,000 shot to lose weight 😏 They’re selling you a cure while your food is laced with “invisible fat” from the water supply. You think this is science? It’s a marketing campaign with a stethoscope. 🤫💉
arun mehta
While I deeply appreciate the clinical depth of this post, I believe the underlying message transcends medical data-it speaks to dignity. Obesity is not a moral failing, nor is it merely a biological malfunction. It is the consequence of systemic neglect: food deserts, wage stagnation, mental health erosion, and the commodification of wellness. Healing requires compassion, not just algorithms and CPAP machines. We must see the person, not the BMI.
Rob Sims
So let me get this straight-after 20 years of being told ‘eat less,’ now we’re supposed to believe a drug that costs $1,000/month is the answer? And you wonder why people are skeptical? You’re just swapping one scam (diet pills) for a bigger one (GLP-1 hype). Wake up.
Sarvesh CK
There is a profound philosophical dimension to this issue that often escapes clinical discourse. The body, in its accumulation of fat, is not merely a site of metabolic dysfunction-it is a mirror of our collective disconnection: from food, from movement, from rest, from community. The triad of diabetes, heart disease, and sleep apnea is not a medical accident; it is the somatic echo of a civilization that has forgotten how to live. To treat these conditions in isolation is to treat symptoms of a deeper wound-the erosion of human rhythm. Perhaps the truest intervention is not pharmaceutical or mechanical, but cultural: rebuilding meals as rituals, movement as joy, and rest as sacred. This is not science fiction. It is ancestral wisdom, waiting to be remembered.