Medication Edema Risk Calculator
Check Your Medication Risk
When to Call Your Doctor
- Sudden swelling in one leg - especially if red, warm, or painful
- Swelling with shortness of breath or chest pain
- Weight gain of more than 2-3 pounds in 24 hours
- Swelling that doesn't improve after stopping medication for a week
- Swelling with confusion or decreased urination
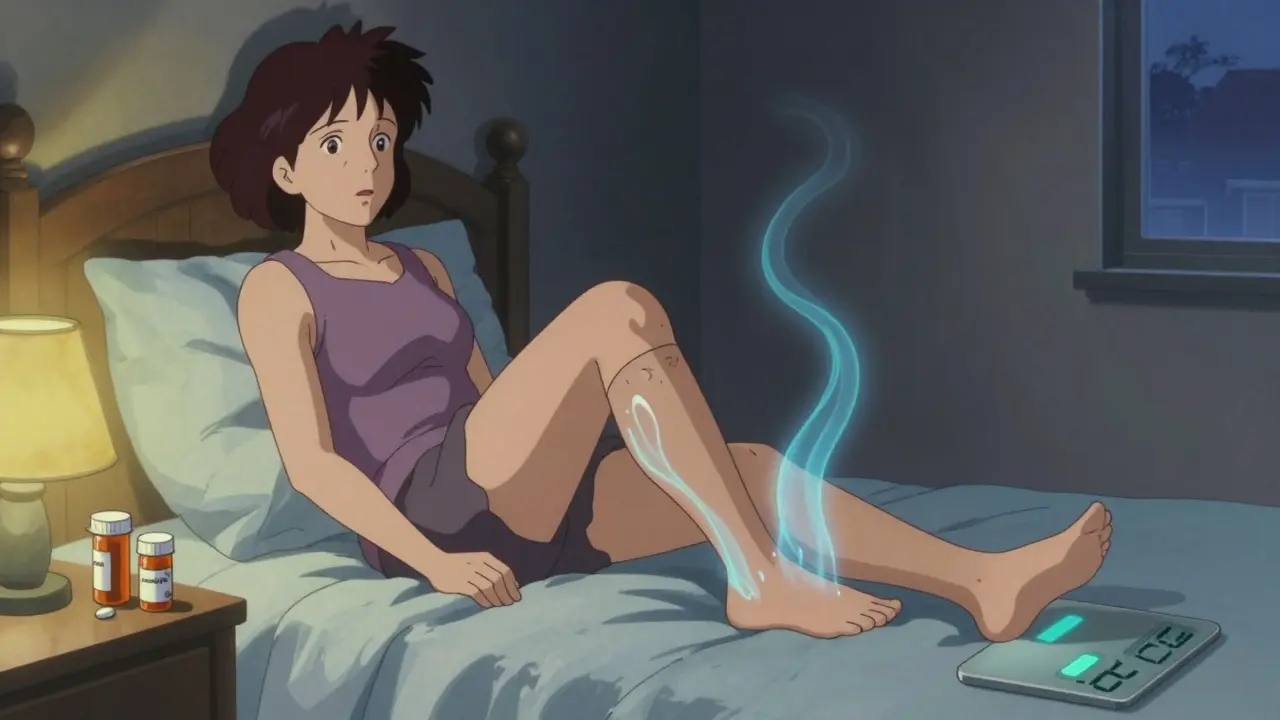
Swelling in your ankles, feet, or hands after starting a new medication isn’t rare - but it’s not always harmless either. You might brush it off as just a side effect, especially if your doctor mentioned it briefly when prescribing the drug. But here’s the thing: medication-induced edema can be a quiet warning sign of something far more serious. In the U.S., over 4 million people experience this every year, and many don’t realize they’re at risk until it’s too late.
What Exactly Is Medication-Related Edema?
Edema is swelling caused by fluid leaking out of tiny blood vessels and building up in your tissues. It’s most common in the legs and ankles - about 75% of all cases show up there. It’s not a disease itself, but a symptom. And when it shows up after you start a new pill, patch, or injection, it’s often linked to the drug you’re taking. Some medications cause this because they change how your body handles salt and water. Others dilate your blood vessels so much that fluid escapes into your skin and muscles. It’s not always obvious which drug is to blame, especially if you’re on multiple prescriptions.Which Medications Are Most Likely to Cause Swelling?
Not all drugs cause edema the same way. Here are the big ones you should know about:- Calcium channel blockers like amlodipine (Norvasc): Used for high blood pressure, they cause swelling in 10-20% of users. At a 10mg daily dose, up to 25% of people notice puffy ankles. Switching to another blood pressure med like losartan often fixes it.
- Gabapentin and pregabalin (Neurontin, Lyrica): These are used for nerve pain and seizures. About 8% of people on gabapentin report noticeable swelling. Patient reviews on Drugs.com give it a 7.8 out of 10 for severity - one of the highest among common prescriptions.
- Thiazolidinediones like pioglitazone (Actos) and rosiglitazone (Avandia): These diabetes drugs cause fluid retention in 4-10% of users. The FDA requires a black box warning on them because they can worsen heart failure. One patient on Reddit shared that their doctor dismissed their swelling until they ended up hospitalized with fluid in their lungs.
- Corticosteroids like prednisone: If you’re taking more than 20mg a day for over two weeks, there’s a 20-30% chance you’ll develop swelling. It’s not just your legs - you might notice your face puffy or your rings tighter.
- NSAIDs like ibuprofen and naproxen: Even common painkillers can cause mild edema in about 3% of regular users. It’s easy to miss because the swelling is small, but it adds up over time.
- Hormonal medications: Birth control pills with 30-35mcg estrogen and hormone replacement therapy with conjugated estrogens can cause fluid retention in 5-15% of users. This is especially common in women over 50.
How to Tell If It’s Just a Side Effect - Or Something Dangerous
Not all swelling is the same. The key is knowing the difference between harmless drug side effects and signs of heart, kidney, or liver problems. Here’s how to tell:- Medication-related swelling is usually bilateral - both legs or both hands. It’s often pitting (you press your finger and it leaves a dent). It tends to get worse by the end of the day and improves overnight.
- Heart failure swelling also affects both legs, but it’s often accompanied by shortness of breath when lying flat (orthopnea), waking up gasping for air (paroxysmal nocturnal dyspnea), or feeling unusually tired. A 2023 American Heart Association report says 90% of advanced heart failure patients have this kind of swelling.
- Kidney disease swelling is usually massive and involves the whole body. You might notice foamy urine, weight gain without eating more, and swelling around the eyes in the morning. Protein loss in urine (over 3.5 grams a day) is a key sign.
- Deep vein thrombosis (DVT) causes swelling in one leg only. The leg might feel warm, red, or tender. This is an emergency - a clot can travel to your lungs.
- Lymphedema after cancer surgery is progressive and doesn’t go down overnight. It’s common after breast cancer treatment, affecting 20-30% of patients who had lymph nodes removed.
When You Should Call Your Doctor Right Away
Don’t wait until the swelling is unbearable. Here are the red flags that mean you need medical attention now:- Sudden swelling in one leg - especially if it’s red, warm, or painful. This could be a blood clot.
- Swelling along with shortness of breath, chest pain, or trouble lying flat. This could mean fluid is building up in your lungs.
- Weight gain of more than 2-3 pounds in 24 hours or 5% of your body weight in a month. That’s a sign your body is holding onto dangerous amounts of fluid.
- Swelling that doesn’t improve after stopping the suspected medication for a week.
- Swelling with nausea, confusion, or decreased urination. This could point to kidney or liver failure.
What You Can Do Right Now
If you’re on a medication that causes swelling and you’re not in immediate danger, here are practical steps you can take:- Elevate your legs above your heart for 15-20 minutes, four times a day. Clinical trials show this reduces ankle swelling by about 1.5cm in just two days.
- Wear compression stockings with 20-30 mmHg pressure. They can reduce swelling volume by 30% in a week.
- Limit sodium to under 2,000mg a day. Most Americans eat over 3,400mg. Cutting salt can shrink swelling in as little as 72 hours.
- Track your weight daily. A 2.2-pound (1kg) jump in a day means your body is retaining fluid. Write it down.
- Don’t stop your meds without talking to your doctor. Some drugs, like blood pressure or diabetes meds, can’t be stopped suddenly.

Why This Matters More Than You Think
Medication-related edema isn’t just annoying - it’s expensive and dangerous. In the U.S., it leads to over 5 million doctor visits a year and costs $4.8 billion in care. Hospitalizations for severe cases run over $11,000 each. Older adults are at higher risk. The American Geriatrics Society lists amlodipine, gabapentin, and pioglitazone as potentially inappropriate for people over 75 because edema risk jumps from 15% under 65 to 40% over 75. New tools are helping. In early 2023, the FDA approved the first wearable device - VascuComp Plus - that uses bioimpedance to detect fluid buildup before it’s visible. Mayo Clinic saw a 22% drop in serious edema cases after adding electronic alerts to their system when patients started high-risk drugs.What to Ask Your Doctor
Next time you see your provider, don’t just accept “it’s just a side effect.” Ask:- “Is this swelling likely from my medication, or should we check my heart or kidneys?”
- “Are there alternatives with less swelling risk?”
- “Should I get a blood test for kidney function or a BNP level to check for heart strain?”
- “Is this something I can manage at home, or do I need to see a specialist?”
Final Thought: Don’t Ignore the Swelling
Swelling from medication isn’t always an emergency - but it’s always a signal. It’s your body saying, “Something’s off.” Ignoring it can lead to hospitalization, worsened heart failure, or missed kidney disease. On the flip side, catching it early means you can switch meds, adjust doses, or start simple fixes like compression socks and salt control - without losing the benefit of the drug you need. You don’t have to live with puffy ankles. You just need to know when to speak up.Can medication swelling go away on its own?
Yes, in some cases. If the swelling is mild and caused by a medication like amlodipine or gabapentin, it may improve after lowering the dose or switching to another drug. Some people see results within a few days to weeks. But if the swelling persists beyond two weeks after stopping the medication, or if it gets worse, you need medical evaluation - it could point to heart, kidney, or liver issues.
Is it safe to take diuretics (water pills) for medication-induced swelling?
Not without medical supervision. Diuretics can help reduce fluid buildup, but they don’t fix the root cause. If your swelling is from heart failure or kidney disease, diuretics might mask the problem. They can also cause electrolyte imbalances, especially if you’re already on blood pressure or diabetes meds. Always talk to your doctor before starting a diuretic.
Why does swelling get worse at the end of the day?
Gravity pulls fluid down into your legs and feet as you stand or sit all day. When you lie down at night, the fluid redistributes - which is why swelling often improves in the morning. This pattern is typical of medication-related and heart-related edema. If swelling stays the same all day or gets worse overnight, that’s a red flag.
Can I prevent medication swelling before it starts?
You can reduce your risk. If you’re starting a drug known to cause swelling - like amlodipine or pioglitazone - ask your doctor about starting at the lowest dose. Keep your sodium intake low, stay active with regular walking, and consider compression socks from day one. Monitoring your weight daily helps catch fluid gain early. Prevention is easier than treating advanced swelling.
Are natural remedies like herbs or supplements helpful for drug-induced swelling?
No reliable evidence supports herbs or supplements for treating medication-induced edema. Some, like dandelion root or hawthorn, are marketed as natural diuretics, but they’re unregulated and can interact with your prescriptions. For example, mixing herbal diuretics with blood pressure meds can cause dangerous drops in blood pressure. Stick to proven methods: elevation, compression, salt control, and medical advice.
Should I stop my medication if I notice swelling?
Never stop a prescribed medication on your own. Stopping blood pressure, diabetes, or seizure meds suddenly can be dangerous - even life-threatening. Instead, call your doctor. They may adjust your dose, switch you to a different drug, or order tests to rule out other causes. Your safety depends on working with your provider, not self-managing.
Gary Hartung
I swear, if I see one more article about 'medication-induced edema' that doesn't mention Big Pharma's profit margins, I'm going to scream. They don't care if your ankles swell-they care if your insurance pays for the next refill. And don't get me started on those 'compression socks'-$80 for a pair of tights that make your legs look like sausages?!
Jason Jasper
I've been on amlodipine for five years. Swelling started slowly. I thought it was just aging. Then I started elevating my legs at night-just propped them on a pillow. Within a week, the puffiness dropped noticeably. No drama. Just simple stuff.
Carlos Narvaez
The data is solid. But let's be precise: calcium channel blockers cause edema via arteriolar dilation, not 'fluid leakage.' And prednisone? That's sodium retention via mineralocorticoid activity. Stop oversimplifying.
Harbans Singh
In India, we don’t always have access to fancy compression socks or bioimpedance devices. But we do know: elevate legs, reduce salt, walk daily. Simple. Cheap. Works. Maybe the West needs to learn from the East sometimes.
Zabihullah Saleh
It’s funny how we treat swelling like a glitch in the system. But what if it’s not a bug-it’s a feature? Your body’s whispering: 'I’m not okay with this.' We’ve forgotten how to listen. We just want a pill to fix the pill. We’re so disconnected from our own biology.
Linda B.
They say it’s 'medication-related'... but have you ever wondered if the FDA approves drugs knowing full well they cause swelling? It’s not an accident. It’s a calculated risk. And you’re the risk. You’re the sacrifice. They’re not testing for your ankles-they’re testing for shareholder returns.
Christopher King
This is just the tip of the iceberg. They pump out drugs like candy, then slap on a tiny warning in 6pt font. And you know what? The real danger isn’t the swelling-it’s that your doctor doesn’t even know the half of it. I’ve seen people on six meds that all cause fluid retention. And they’re told to 'just take a diuretic.' Like that’s a solution. It’s a Band-Aid on a severed artery.
Michael Dillon
I’m not saying you’re wrong, but have you considered that maybe the swelling isn’t from the meds at all? Maybe it’s your diet? Or your job? Or you’re just sitting too much? I’ve seen people blame amlodipine when they’re eating 100g of sodium a day and never move from their couch.
Justin James
I’ve been researching this for years. The real issue isn’t the drugs-it’s the gut microbiome. When you take meds, they alter your gut flora, which triggers systemic inflammation, which leads to capillary permeability, which causes edema. No one talks about this because the pharmaceutical industry doesn’t profit from probiotics. They want you dependent on drugs, not healing your gut. The data is out there-if you know where to look.
Winni Victor
I started gabapentin last month. My ankles looked like overinflated balloons. I cried. I yelled. I threw my socks across the room. Then I ate a whole pizza. And guess what? The swelling didn’t get worse. So maybe it’s not the meds. Maybe it’s just… me. And my emotional relationship with gravity.
Rick Kimberly
The clinical evidence presented is methodologically sound. However, one must consider confounding variables: age, renal function, concomitant medications, and baseline albumin levels. The 2023 AHA guidelines emphasize differential diagnosis before attributing edema solely to pharmacologic agents. I recommend formal evaluation before self-intervention.
Terry Free
You people are so dramatic. Swelling? Big deal. My grandma took prednisone for 20 years and still gardened. You’re not sick-you’re lazy. Stop whining. Eat less salt. Move your legs. Stop expecting the world to fix your laziness with a new pill.
Ben Harris
I just want to say I’m not mad-I’m just disappointed. I trusted my doctor. I took the pills. I didn’t ask questions. And now I can’t fit into my shoes. And no one told me. No one warned me. I just thought I was getting fat. I’m not fat. I’m full of poison.