BPPV and Why the Room Starts Spinning: What’s Really Going On?
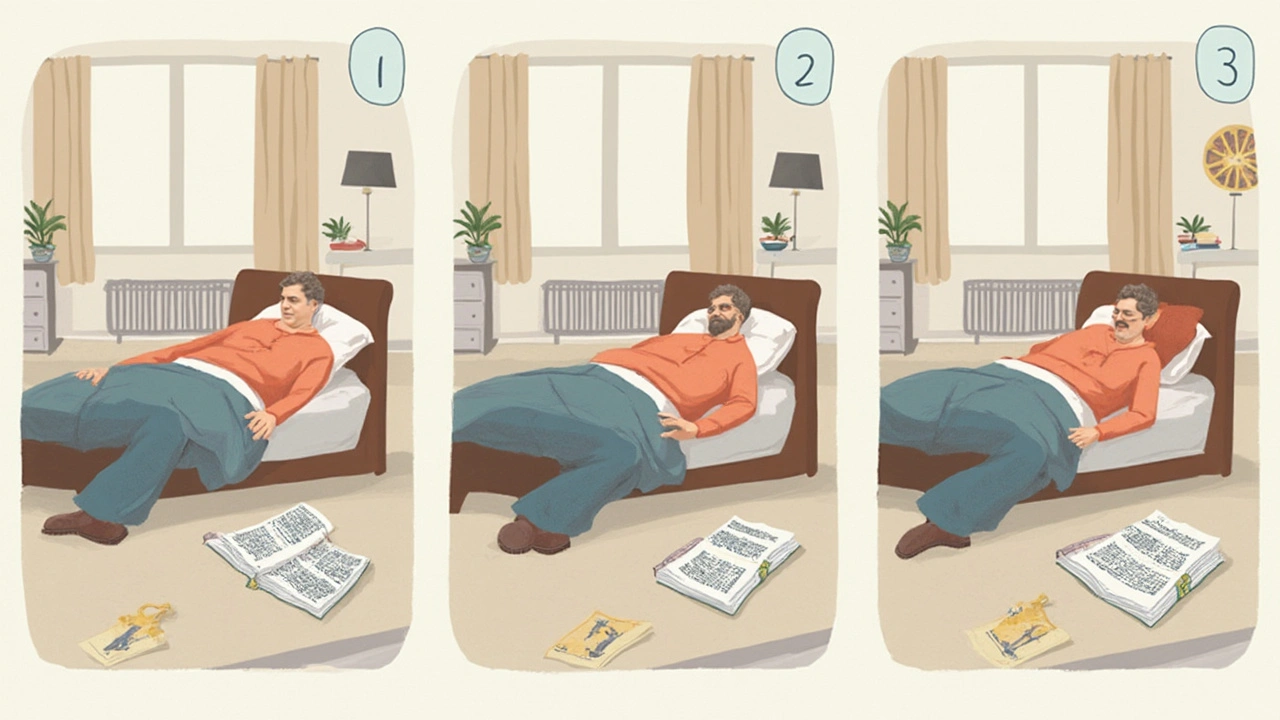
If you’ve ever rolled over in bed and felt the whole room whirl like a carnival ride, you know why BPPV (benign paroxysmal positional vertigo) can be so unsettling. BPPV is all about signals gone rogue in your inner ear. Those tiny calcium crystals (called otoconia) that help with balance sometimes float into places they don’t belong—mainly the semicircular canals. Once they’re out of place, every little head movement tricks your brain into thinking you’re spinning, even if you’re lying perfectly still. For some people, these dizzy spells are quick but intense, lasting less than a minute, but returning again and again.
I remember when my son Liam had his first full-blown BPPV attack. He looked at me with wide eyes and said, “Dad, did the house just tip?” He was convinced gravity had changed. But no, it was just those little crystals making mischief. Millions of adults—especially folks past 40—deal with BPPV at some point, but a surprising number of younger kids can get it, too. Each episode feels random, but it usually flares up after fast head turns, lying down, or even just looking up. Medical research says BPPV is not dangerous, but it can definitely mess up your routine. Driving, cooking, even walking down the hall can suddenly feel like Olympic sports.
Doctors can usually spot BPPV with a quick set of eye movement tests. They might make you lie back or turn your head sharply to see if your eyes jump (nystagmus, if we want to get technical). Most times, tests and scans aren’t needed. But the real trick is not just surviving the spins—it’s learning to stop them or at least dial them down. That’s where home maneuvers and certain medications come in.
How Meclizine Helps with the Vertigo — and What It Can't Do
The first instinct when dizziness strikes is often to reach for medicine. Meclizine has become the go-to over-the-counter option for dizzy spells, especially with BPPV. It’s an antihistamine, but not the stuff you take for a runny nose. Meclizine basically calms down the signals coming from your inner ear, making your brain less likely to send out those “You’re spinning!” alerts. So instead of the bed feeling like a tilt-a-whirl, things get way less dramatic—sometimes just a gentle wobble.
But here’s where it’s interesting: meclizine doesn’t fix the actual cause. It doesn’t move the rogue calcium crystals back where they belong. That means you’re only taking the edge off the dizziness for a while. Think of it like dimming the lights instead of fixing the blown bulb. The latest research even shows that some people find meclizine works better when they use it just at the peak of an attack, not daily. Talk to your doctor about what makes sense for you. Drowsiness is the big side effect; take it and you may feel like you pulled an all-nighter. Other people complain of dry mouth or a fuzzy head. My neighbor actually fell asleep in the movie theater after a dose. So, don’t drive or do anything risky right after using it.
Here’s something most people don’t realize: overusing meclizine for BPPV can sometimes mask symptoms of more serious problems like migraine or stroke. If the dizziness is new, terrifying, or comes with slurred speech or weakness, you need more than just a pill. Also, kids under 12 shouldn’t use meclizine unless told by their doctor. Always read the dosing directions carefully and ask about interactions if you take other medicines for allergies, anxiety, or blood pressure.
When meclizine works, it usually starts calming dizziness within an hour. That’s fast relief if you’re stuck sitting at your desk hoping nobody notices your head resting on your keyboard. The effects can last up to 24 hours, though most people say they feel a little foggy during that time. If you’re using it more than a few days in a row, or if it seems to stop working, it’s time to call your doctor for new ideas. People who are pregnant, breastfeeding, or older adults—especially those worried about falls—need to be even more careful with dosing. The medication can add to other sleepy or dizzy sensations, so be honest with your doc about everything you take, even vitamins. They appreciate those details more than you think.
Mastering the Epley Maneuver: Crystal Clearing at Home
Swallowing a pill is easy, but the real BPPV game-changer is the Epley maneuver. This home exercise can sometimes cure vertigo in minutes by moving loose crystals back to their rightful spot in your ear. The trick is doing it slowly and following the exact steps. My advice? It’s way easier with a friend the first time—Liam still giggles about trying it with me, especially because you might end up in some funky head positions.
Doctors have taught the Epley maneuver for decades, but you don’t need any special equipment—just a flat surface and a bit of patience. Here’s how it works if your right ear is the troublemaker. (You can reverse the steps for the left.)
- Sit on the edge of your bed, turn your head 45 degrees to the right (or left, for the other ear).
- Quickly lie down on your back so your head hangs slightly off the edge, still turned. Wait 30-60 seconds, or until any spinning stops.
- Slowly turn your head 90 degrees to the left, letting it rest that way, and wait another 30-60 seconds.
- Turn your whole body another 90 degrees in the same direction, rolling until you’re staring at the floor. Rest here for another half-minute.
- Sit up slowly, keeping your chin tucked in. Stay upright for a few minutes.
Sounds awkward? It is, the first couple times. But studies show the Epley maneuver works for about 80% of people with classic BPPV. The key is not rushing and not getting discouraged. If the spinning worsens, or if you’re not sure what to do, get a physical therapist or doctor to walk you through it the first time. There are lots of videos online, but stick to ones put out by major hospitals or neurologists.
Some people wonder if they can do both—the Epley and meclizine—on the same day. Sure, but it’s usually smart to only take meclizine if you absolutely need it, like when things get way too miserable to function. Don’t do the Epley right after a big meal or when you’re feeling sleepy from meds, or you’ll risk a stomachache and maybe a nap you didn’t plan for.
Tips for Staying Safe with Meclizine and BPPV Maneuvers
Managing vertigo isn’t just about what you take or which moves you try—it’s about the daily little choices. Keep a simple log of when you get dizzy spells. I once made a spot in my phone notes for Liam’s episodes, jotting down what he ate, how much water he drank, and if he bumped his head at recess. Sometimes there’s no pattern, but sometimes you spot triggers like dehydration, sudden head turns, or even stressful days at work or school.
Here are some real-world ways to make life less wobbly while managing BPPV and taking meclizine:
- Stay hydrated—being even a little dehydrated can make vertigo worse.
- If you’re new to meclizine, try it at home first, where you can sit or lie down comfortably.
- Set alarms for doses—meclizine makes some folks forgetful.
- Avoid caffeine and nicotine on vertigo days; both can make symptoms worse.
- Use extra pillows to prop your head up in bed, or sleep slightly reclined for a while.
- Get up slowly in the morning. Sit first, then stand. Don’t sprint to the coffee pot!
- Clear the path in your bedroom and bathroom of trip hazards, especially in the days right after a bad dizzy spell.
- Let someone know when you’re about to do the Epley maneuver, just in case you feel woozy and need help sitting up.
- Teach kids in the family what to do if they see you stumbling or sitting suddenly—kids love to be the "helper," and it gives everyone peace of mind.
- Never combine meclizine with alcohol or sedating meds unless a doctor says it’s okay.
- Ask your doctor before flying or going on a rollercoaster while you’re still getting BPPV flares.
Safety’s not just about avoiding falls. If you notice hearing loss, double vision, severe headache, or numbness on one side, forget the meclizine and call for help—these are not typical BPPV symptoms. If you’re caring for someone older, remember that they may downplay their dizziness out of pride or fear of losing independence, but being honest saves a lot of drama.
Some surprising data: a 2022 review in a leading neurology journal found that simple home strategies—like sleeping on the “good” side, gentle yoga without wild head moves, and focusing on a spot while standing—cut down on daily dizzy spells almost as much as medication for some folks. Little changes make a big dent.
The balancing act with BPPV and meclizine is all about knowing your body and not pretending you’re invincible. Whether it’s you or your kid waking up to a spinning ceiling, you’ve got tools to fight back—you just have to use them smartly.

Jenny Spurllock
I’ve noticed that the timing of meclizine’s onset can vary quite a bit between individuals, so keeping a simple log of when you take the dose and when the spin eases can really help you and your doctor fine‑tune the schedule. Also, staying hydrated before taking the pill seems to reduce the feeling of fog that some people report. It’s a small habit that’s easy to adopt.
Bart Cheever
Meclizine works, but it isn’t a cure. The maneuver is still required.
Maude Rosièere Laqueille
When you combine a short course of meclizine with a properly performed Epley maneuver, you’ll often notice the dizziness fades faster than with either approach alone. The medication can blunt the vertigo enough to let you focus on the head positioning without the overwhelming sensation of spinning. Just be sure to take the pill at least an hour before you start the series of movements so the sedative effect has settled. If you feel overly drowsy, pause the maneuver and rest for a few minutes before continuing. Documenting both the dose time and the maneuver steps in the same log gives your clinician a clear picture of what works best for you.
Amanda Joseph
Ehh, sure, because popping a sleepy pill always makes you a ninjA.
Kevin Aniston
First, let me say that dealing with BPPV is a marathon, not a sprint, and the tools we have-meclizine and the Epley maneuver-are like the water and shoes you need for the race. You start by acknowledging that the medication gives you a temporary window of clarity; during that window you can safely perform the repositioning steps without the intrusive sensation of the world spinning. Next, keep a detailed diary: note the exact time you take meclizine, the time you begin the maneuver, and any residual symptoms you feel afterwards. Over the course of a week, patterns emerge-perhaps you notice that taking the pill an hour before bedtime reduces nighttime vertigo, or that doing the maneuver right after a light snack prevents stomach discomfort. It’s also worth mentioning that hydration plays a silent but crucial role; dehydration can amplify the otolithic instability, making both the drug and the maneuver feel less effective. If you ever feel the side‑effects of meclizine, such as excessive drowsiness or a dry mouth, pause the medication for a day and rely solely on the repositioning technique to see if you can maintain balance without pharmacologic aid. For those who experience frequent recurrences, a referral to a vestibular physiotherapist can fine‑tune the maneuver to your specific canal involvement, sometimes requiring a modified version of the Epley or the Semont technique. Additionally, avoid sudden head movements for at least 24‑48 hours after a successful maneuver; even a quick glance up can toss the crystals back into the canal. Finally, keep your doctor in the loop-share your log, discuss any lingering fog, and ask about alternative antihistamines if meclizine’s sedation becomes a roadblock. In my experience, this systematic approach turns a chaotic series of dizzy spells into a predictable, manageable routine, and most patients report a marked reduction in both frequency and severity after a few weeks of disciplined practice.
kiran kumar
i cant believe people keep popping pills like candy it’s just a band aid for a problem that needs real work the crystals dont move themselves you gotta do the thing not just chill and hope it fixes itself
Brian Johnson
I get where you’re coming from, and it’s easy to feel frustrated when quick fixes seem tempting. Still, taking a moment to actually perform the recommended maneuvers can give you lasting relief that a pill alone can’t provide. Staying hydrated and keeping a log of episodes also helps you spot triggers before they turn into full‑blown spins. If you ever feel uncertain, a brief check‑in with a vestibular therapist can clear up any doubts.
Jessica Haggard
Absolutely, staying proactive is the best defense. I always tell friends to combine a low dose of meclizine with the Epley only when the vertigo spikes, so they stay alert for daily tasks. It’s also smart to clear the hallway of shoes and toys before attempting the maneuver-safety first, fun second. And don’t forget to let your family know what to look for if you suddenly lose balance; their help can prevent a nasty fall.
Alan Clark
Hey folks, just wanted to say that even if you’re skeptical, giving the Epley a try with a friend nearby can turn a scary moment into a team effort. Most people see improvement within a few tries, and the sense of control feels amazing. Keep the vibes positive and the head steady!