Acetaminophen and NSAIDs aren’t the same - and picking the wrong one can make your pain worse or hurt your health.
You’ve got a headache. Your knees ache after gardening. Your period cramps hit hard. You reach for the medicine cabinet. But which bottle do you grab? Acetaminophen or an NSAID? It’s not just a brand choice - it’s a medical decision. And most people don’t know the difference.
Acetaminophen (sold as Tylenol, Panadol, and store brands) and NSAIDs (like ibuprofen, naproxen, and aspirin) both reduce pain and fever. But that’s where the similarity ends. One works mostly in your brain. The other works everywhere - including your stomach, heart, and joints. And that changes everything.
How acetaminophen actually works - and when it’s your best bet
Acetaminophen doesn’t touch inflammation. That’s key. It doesn’t reduce swelling, redness, or warmth in a sore joint. Instead, it quietly blocks pain signals in your brain and spinal cord. Think of it like turning down the volume on pain, not fixing the source.
This makes it ideal for headaches, mild back pain, and fever. The Mayo Clinic says 70% of people with migraines find relief with acetaminophen. It’s also the only OTC pain reliever recommended for children under 12 and pregnant women, according to University of Utah Health guidelines from 2023.
It’s gentle on the stomach. You can take it on an empty stomach without worrying about ulcers. That’s why doctors often suggest it as a first step. Harvard Health calls it "pretty well-tolerated with or without food." And it’s cheap - generic acetaminophen costs as little as $0.03 per 500mg tablet.
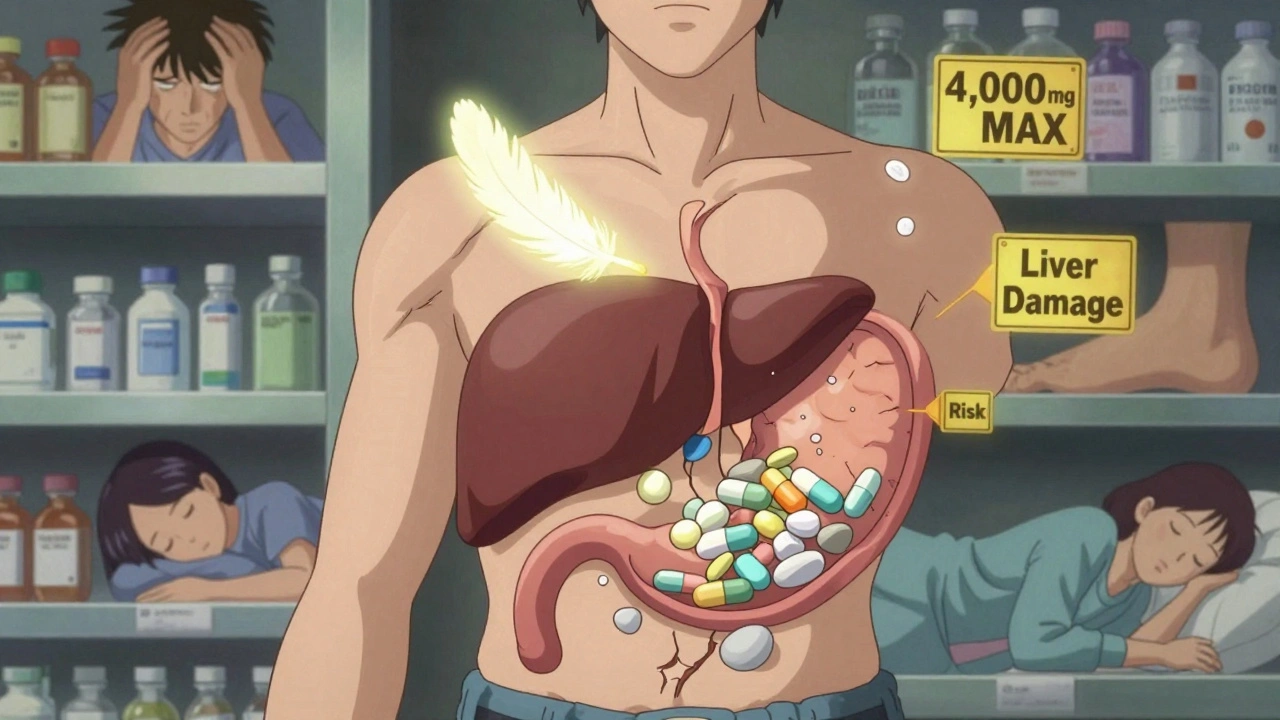
But here’s the catch: your liver pays the price. The maximum daily dose is 4,000 mg - but experts now advise sticking to 3,000 mg or less. Why? Because liver damage can happen even within the "safe" range. The CDC reports 15,000 hospitalizations a year from acetaminophen overdose. Most of those? People didn’t realize they were doubling up - taking Tylenol for a headache and a cold medicine that also had acetaminophen. The FDA now requires bright red warnings on every bottle for this reason.
How NSAIDs work - and why they’re better for swollen, inflamed pain
NSAIDs - nonsteroidal anti-inflammatory drugs - work differently. They block enzymes called COX-1 and COX-2 that produce prostaglandins. These chemicals cause pain, fever, and inflammation. So NSAIDs don’t just mask pain - they fight the swelling behind it.
That’s why they’re the go-to for arthritis, tendonitis, sprains, and menstrual cramps. American Academy of Family Physicians (AAFP) research shows NSAIDs reduce osteoarthritis pain by 30-50%, while acetaminophen only helps by 10-20%. For a swollen knee, NSAIDs win. Hands down.
Common NSAIDs include:
- Ibuprofen (Advil, Motrin): Dose every 4-6 hours. Max 1,200 mg/day OTC.
- Naproxen (Aleve): Lasts longer - up to 12 hours per dose. Max 660 mg/day OTC.
- Aspirin: Also an NSAID, but less used for pain now due to bleeding risks.
Naproxen has a slight edge over ibuprofen for heart safety. A 2021 study in the European Heart Journal found naproxen carries a lower risk of heart attack than ibuprofen. That’s why some cardiologists prefer it for people with mild heart concerns.
The big trade-off: stomach safety vs. inflammation control
NSAIDs are great for swelling - but they’re hard on your gut. Every year, 2-4% of regular NSAID users develop stomach ulcers. That’s 1 in 25 people. The risk goes up with age, alcohol use, or taking them for more than a few days straight.
Acetaminophen? Less than 0.5% risk of ulcers. That’s why Harvard Health recommends it as the first choice for most mild pain - especially if you’ve ever had stomach issues.
But here’s the twist: if you have arthritis, osteoarthritis, or a sprained ankle, skipping NSAIDs means you’re missing the root cause. Pain relief without reducing inflammation is like turning off an alarm without fixing the fire.
Want to protect your stomach while using NSAIDs? Take them with food. Or ask your doctor about adding famotidine (Pepcid), which reduces acid. Never mix NSAIDs - no ibuprofen + naproxen. That triples your risk of internal bleeding, according to the FDA.
Who should avoid each drug - and who should use them with caution
Some people simply shouldn’t take one or the other.
Avoid acetaminophen if:
- You drink 3+ alcoholic drinks a day
- You have liver disease
- You’re taking other meds with acetaminophen (cold, flu, or sleep aids)
Avoid NSAIDs if:
- You have a history of stomach ulcers or bleeding
- You have heart disease, high blood pressure, or kidney problems
- You’re over 65
- You’re taking blood thinners like warfarin
The American Heart Association now advises people with established heart disease to avoid NSAIDs unless absolutely necessary. Ibuprofen raises heart attack risk by 10-50% with long-term use, per FDA warnings from 2021. Naproxen is a safer option here - but still not risk-free.
For pregnant women: acetaminophen is safe in all trimesters. NSAIDs? Avoid after 20 weeks. They can affect fetal kidney development and reduce amniotic fluid.
For kids: acetaminophen is the only recommended OTC painkiller for babies under six months. For older children, both are options - but always use weight-based dosing (10-15 mg/kg per dose for acetaminophen).
Can you take them together? Yes - and here’s how to do it safely
Here’s something most people don’t know: combining acetaminophen and an NSAID can give you better pain relief than either one alone - with lower doses of each. That means fewer side effects.
Harvard Health specifically recommends this approach. For example: take 650 mg of acetaminophen and 200 mg of ibuprofen at the same time. Wait 4-6 hours before repeating. You’re getting the anti-inflammatory power of the NSAID plus the brain-focused pain blocking of acetaminophen.
But here’s the rule: never take two NSAIDs together. And never exceed the daily max for either drug. Track your doses. Use a phone app or a paper log. People who overdose on acetaminophen often do it by accident - they don’t realize their nighttime cold medicine has it too.

What’s the bottom line? Pick based on your pain - not the brand
Need relief from a headache, fever, or mild muscle ache? Start with acetaminophen. It’s gentle, cheap, and safe for most people - including pregnant women and kids.
Got swollen joints, a sprained ankle, or painful periods? Go with an NSAID. Naproxen lasts longer. Ibuprofen works faster. Both reduce inflammation - which acetaminophen simply can’t do.
And if your pain is stubborn? Try both - but space them out and stick to the limits. This isn’t about being "stronger" - it’s about being smarter.
Remember: OTC doesn’t mean harmless. These are real drugs with real risks. The labels aren’t there for show. Read them. Know your limits. And if pain lasts more than a few days - see a doctor. There’s probably a reason it won’t go away.
What about long-term use? Should you be worried?
For most people, occasional use of either drug is fine. But daily use? That’s where things get risky.
Long-term acetaminophen use - even at 3,000 mg/day - can slowly damage the liver, especially if combined with alcohol or other medications. There’s no warning sign until it’s too late.
Long-term NSAID use? That’s linked to kidney damage, high blood pressure, and heart problems. The NIH is currently funding 17 clinical trials to find safer alternatives - but none have replaced these drugs yet.
Both will remain first-line OTC options through 2030, according to Harvard Medical School. Why? They work. They’re cheap. And we know how to use them - if we’re careful.
Is acetaminophen safer than ibuprofen?
It depends on what you’re comparing. Acetaminophen is safer for your stomach and kidneys, and it’s the only OTC pain reliever recommended for pregnant women and young children. But ibuprofen is safer for your liver - and far more effective for inflammation. If you have a history of ulcers or liver disease, acetaminophen is usually the better pick. If you have arthritis or swelling, ibuprofen works better - as long as you don’t have heart or kidney issues.
Can I take acetaminophen and ibuprofen together?
Yes - and it’s often recommended. Taking 650 mg of acetaminophen with 200 mg of ibuprofen at the same time can give you stronger pain relief than either alone, while lowering the risk of side effects. Just make sure you don’t exceed the daily maximum for either drug (3,000 mg for acetaminophen, 1,200 mg for ibuprofen). Don’t take them more than every 4-6 hours, and never combine with other pain meds that contain either ingredient.
Which is better for arthritis: acetaminophen or NSAIDs?
NSAIDs are significantly better for arthritis. Studies show they reduce pain by 30-50% in osteoarthritis patients, while acetaminophen only helps by 10-20%. That’s because arthritis involves inflammation - and acetaminophen doesn’t reduce inflammation. If your joints are swollen, warm, or stiff, NSAIDs like naproxen or ibuprofen are the clear choice. Acetaminophen might help a little with the pain, but it won’t fix the swelling.
Why does Tylenol have a liver warning and Advil has a heart warning?
Because they affect different organs. Acetaminophen is processed by the liver, and too much can cause serious liver damage - even at recommended doses if you drink alcohol or take other meds. That’s why the FDA required stronger liver warnings in 2011. NSAIDs block enzymes that protect the stomach lining and regulate blood flow, which can lead to ulcers, kidney issues, and increased heart attack risk - especially with long-term use. The FDA mandated heart warnings on NSAID labels in 2015 after studies showed a clear link to cardiovascular events.
Is naproxen safer than ibuprofen?
For heart safety, yes. A 2021 study in the European Heart Journal found naproxen carries a lower risk of heart attack than ibuprofen. It also lasts longer - one dose can work for up to 12 hours. But both can cause stomach ulcers. If you have heart disease or high blood pressure, naproxen is usually the preferred NSAID. But if you need fast relief and have no heart issues, ibuprofen works fine. Always take the lowest effective dose for the shortest time.
Can I use OTC pain relievers every day?
Not without talking to a doctor. Daily use of acetaminophen can damage your liver over time. Daily NSAID use increases your risk of ulcers, kidney problems, and heart events. If you’re taking either every day for more than 10 days, you should see a provider. Chronic pain isn’t something you should manage with OTC pills alone. There could be an underlying condition - like arthritis, nerve damage, or an autoimmune issue - that needs a different treatment.
What to do next if your pain doesn’t improve
If you’ve tried the right medication - acetaminophen for headaches, NSAIDs for swelling - and your pain hasn’t improved after 3-5 days, it’s time to see a doctor.
Don’t just crank up the dose. Don’t mix more pills. Don’t assume it’s "just aging." Pain that lingers is your body’s signal that something’s wrong.
Keep a simple pain log: what hurt, when, how bad (1-10 scale), what you took, and whether it helped. Bring that to your appointment. It tells your doctor more than you think.
There are better options than OTC pills for chronic pain - physical therapy, targeted injections, nerve blocks, even lifestyle changes. But you won’t find them if you keep reaching for the same bottle.

Josh Bilskemper
Acetaminophen is literally just a placebo with a liver tax. If you're taking it for anything beyond a mild headache, you're deluding yourself. NSAIDs are the only real option. Period.
Stop pretending it's 'gentle'-it's just ineffective.
Storz Vonderheide
I appreciate how thorough this breakdown is. I'm from Nigeria and we don't always have access to the same meds, but the liver vs. stomach trade-off is universal. My uncle took ibuprofen daily for years and ended up with a bleed-he didn't know it was linked. This kind of clarity saves lives.
dan koz
Bro you just described my entire life. Headache? Tylenol. Knee pain? Advil. But I mix them like a pro-650 and 200, every 6 hours. No issues. My grandma says I'm reckless. I say I'm optimized.
Kevin Estrada
I JUST GOT DIAGNOSED WITH EARLY ARTHRITIS AND I WAS TAKING TYLENOL FOR 3 YEARS. I'M SO MAD. I COULD'VE BEEN TAKING NAPROXEN THIS WHOLE TIME. MY KNEES ARE A MESS NOW. THIS POST IS A TRAGEDY AND A REVELATION. I'M CRYING.
Also I think Tylenol is for people who are scared of pain. Like... why not just feel it?
Michael Bene
The real villain here isn't acetaminophen or NSAIDs-it's Big Pharma's marketing machine. They sell Tylenol as 'the gentle giant' while burying the liver stats in tiny print. Meanwhile, Advil gets slapped with a heart warning like it's a horror movie trailer. Meanwhile, naproxen? The quiet overachiever nobody talks about. It's the Swiss Army knife of OTC painkillers-long-lasting, lower cardiac risk, and still gets the job done. Why isn't this on every bottle? Because they want you to buy more bottles.
kelly mckeown
i read this and thought of my mom. she takes tylenol every day for her back and never tells anyone. i’m gonna print this out and leave it on her fridge. she’s 72 and doesn’t trust doctors. but she trusts facts. thank you for writing this so clearly.
Tom Costello
This is one of the most balanced, well-sourced OTC pain guides I’ve seen in years. The part about combining acetaminophen and NSAIDs? That’s gold. I’ve been doing that for my chronic lower back pain for 2 years-650 mg + 200 mg every 6 hours. No stomach issues, no liver spikes. My PCP was skeptical until I showed him my bloodwork. Turns out, smart stacking works.
dylan dowsett
Wait-so you’re telling me I’ve been taking Advil for my period cramps for 15 years... and I could’ve been using naproxen? And I didn’t know that acetaminophen doesn’t touch inflammation? Are you serious? I’ve been treating symptoms like a toddler with a hammer. I’m embarrassed. And now I’m mad at every pharmacist who never explained this.
Susan Haboustak
This article is dangerously oversimplified. You mention '3,000 mg/day' as safe, but the CDC says liver damage occurs in 10% of chronic users even below that. You say naproxen is 'safer for the heart'-but the European Heart Journal study had a 0.8% absolute risk difference. That’s not 'safer,' it’s marginally less dangerous. And you completely ignore the fact that NSAIDs increase blood pressure in 30% of users. This isn't education. It's wellness influencer nonsense dressed as medical advice.
Chad Kennedy
I took ibuprofen for my back for 6 months straight. Then I got dizzy. Then I threw up blood. Then I went to the ER. They said 'you're lucky you didn't die.' Now I just lie on the floor and cry. Tylenol doesn't work. But at least I'm alive. So... I guess that's something?
Siddharth Notani
Excellent summary. 🙏 For those in India, generic naproxen (500mg) costs ₹5 per tablet. Acetaminophen is ₹3. But always consult a physician before daily use. Your body is a temple. 🕉️
Cyndy Gregoria
You guys are overcomplicating this. If it hurts, try one. If it doesn’t help, try the other. If both fail, see a doctor. Don’t overthink it. Your body knows. Listen to it. And stop taking pills like candy. You’re not a superhero. You’re a human. Rest. Hydrate. Move. Sometimes the medicine is just the backup plan.