High cholesterol isn’t something you feel. No pain. No warning signs. No sudden dizziness. That’s why it sneaks up on so many people-until it doesn’t. By the time symptoms show up, the damage is often already done. Hypercholesterolemia, the medical term for high cholesterol, is quietly building up plaque in your arteries, inch by inch, year after year. It’s not just a number on a lab report. It’s a silent countdown to heart attack, stroke, or early death.
What Exactly Is Hypercholesterolemia?
Hypercholesterolemia means your blood has too much cholesterol-specifically, too much low-density lipoprotein, or LDL. This is the "bad" cholesterol that sticks to artery walls, forming fatty deposits called plaques. Over time, these plaques harden and narrow your arteries, making it harder for blood to flow to your heart and brain.
The American Heart Association says about 93 million U.S. adults have total cholesterol above 200 mg/dL. That’s nearly 40% of the adult population. But not all high cholesterol is the same. There are two main types: familial (genetic) and acquired (lifestyle-driven).
Familial hypercholesterolemia (FH) is inherited. You’re born with it. If one parent has FH, you have a 50% chance of getting it. About 1 in 250 people worldwide have this condition. People with FH often have LDL levels over 190 mg/dL from childhood. Some even hit 400-500 mg/dL. These individuals are at extreme risk-untreated, they can have heart attacks in their 30s or 40s. Men with FH often have their first cardiac event by 53. Women, by 60.
Acquired hypercholesterolemia, on the other hand, comes from diet, inactivity, or other health issues like diabetes, hypothyroidism, or kidney disease. It’s more common. And it’s often reversible-if you act early.
How Do You Know If You Have It?
You don’t. Not unless you get tested.
There are no physical symptoms in the early stages. No headaches. No fatigue. No stomach issues. The only way to know is through a simple blood test called a lipid panel. The U.S. Preventive Services Task Force recommends screening for all adults between 40 and 75. But if you have a family history of early heart disease, or if you’re overweight, diabetic, or smoke, you should get tested earlier-even in your 20s.
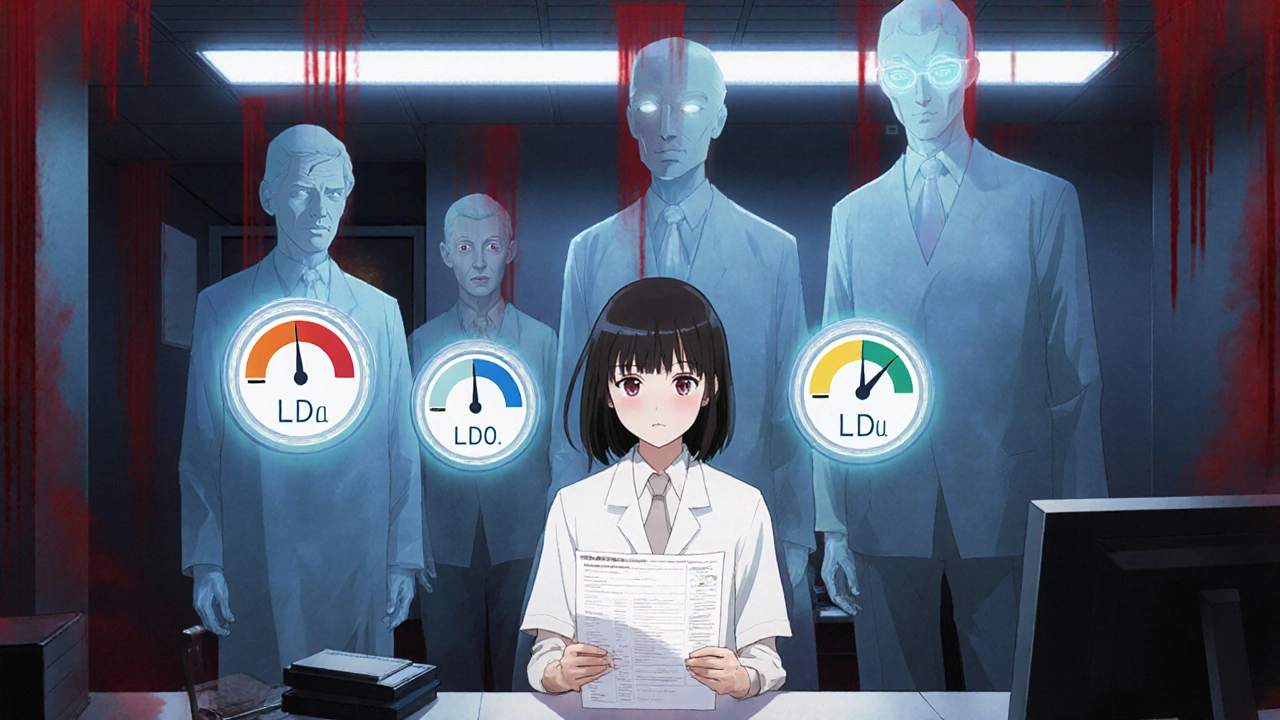
The test measures:
- Total cholesterol
- LDL (bad cholesterol)
- HDL (good cholesterol)
- Triglycerides
Here’s what the numbers mean:
- Desirable LDL: under 100 mg/dL
- Borderline high: 130-159 mg/dL
- High: 160-189 mg/dL
- Very high: 190 mg/dL or above
Severe hypercholesterolemia? That’s LDL over 190. If you’re in that range, especially without obvious lifestyle causes, you could have FH. Look for physical signs: yellowish bumps around the eyes (xanthelasmas), or thickened tendons in your heels or knuckles (tendon xanthomas). These are telltale signs of genetic cholesterol problems.
Why Does It Matter So Much?
High cholesterol doesn’t just raise your risk of heart disease-it makes it inevitable if left alone. According to the World Health Organization, cardiovascular diseases kill 17.9 million people every year. That’s more than cancer. And high cholesterol is the top driver.
Every 39 mg/dL drop in LDL cuts your risk of heart attack, stroke, or death by 22%. That’s not a small number. That’s life-changing. A 2022 study in the Journal of the American College of Cardiology confirmed it: aggressive LDL lowering saves lives.
And it’s not just about the heart. Clogged arteries mean less blood flow to the brain. That’s how strokes happen. Less blood to the legs? That’s peripheral artery disease. Less blood to the kidneys? That’s kidney damage. Cholesterol doesn’t just sit in one place. It spreads.
People with untreated familial hypercholesterolemia lose about 30 years of life expectancy. That’s not an exaggeration. It’s data from the European Atherosclerosis Society.
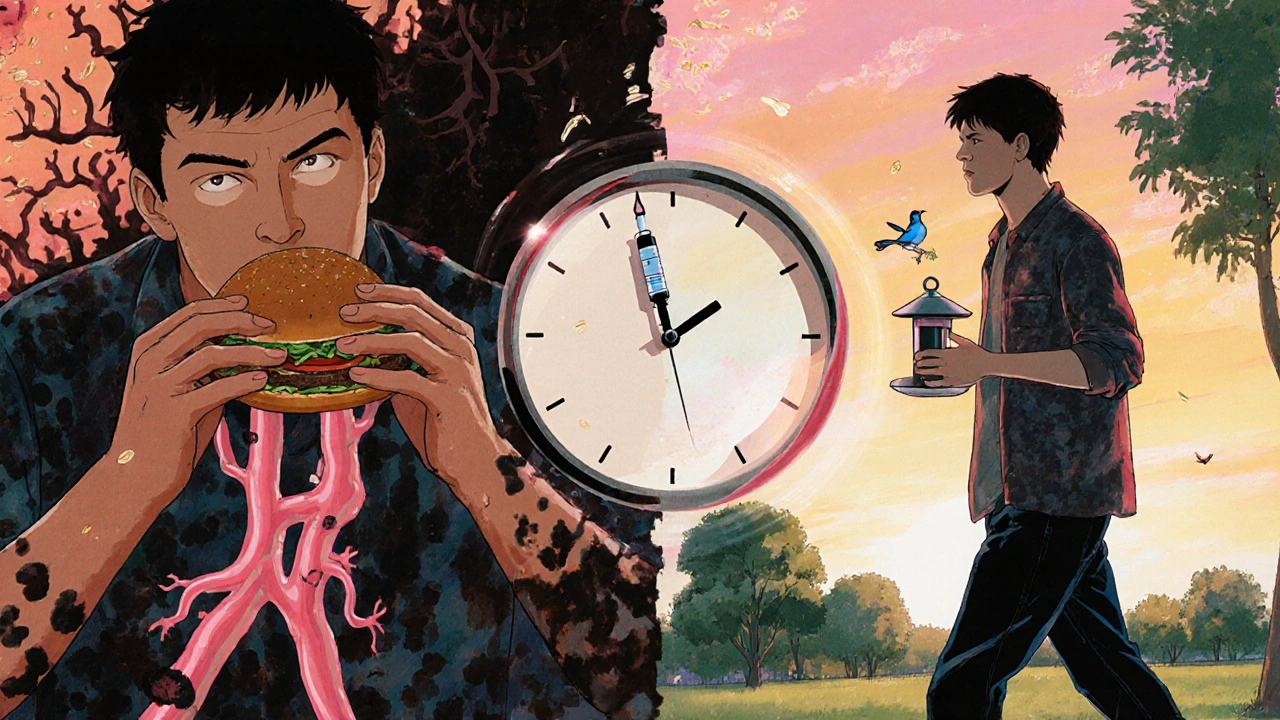
Genetic vs. Lifestyle: What’s the Difference?
Here’s the big divide: genetics vs. choices.
If you have familial hypercholesterolemia, no amount of salads or yoga will fix it. Your body can’t clear LDL properly because of a broken gene-usually in the LDLR or PCSK9 gene. You need medication, and you need it early. Often, you’ll need a combo of three drugs: a high-dose statin, ezetimibe, and a PCSK9 inhibitor like evolocumab. These drugs can slash LDL by 60% or more.
But if your high cholesterol comes from eating too many fried foods, skipping exercise, or being overweight, the story changes. You can reverse it. The Portfolio Diet-rich in oats, nuts, plant sterols, soy, and fiber-has been shown in clinical trials to lower LDL by 10-15% on its own. Combine that with weight loss and daily walking, and you can cut LDL by 30% or more without a single pill.
Here’s the catch: lifestyle changes require consistency. Most people stick with diet changes for six months. After a year? Only 45% are still doing it. That’s why medication works better for some. It’s easier to take a pill than to resist pizza every night.
How Is It Treated?
Treatment starts with two things: testing and talking.
Step 1: Get your numbers. No fasting needed anymore. Most labs can test cholesterol without it.
Step 2: Figure out why. Is it genetic? Is it diabetes? Are you on a medication that raises cholesterol, like certain blood pressure pills?
Step 3: Set a goal. The 2018 AHA/ACC guidelines say high-risk patients should aim for at least a 50% drop in LDL. The European guidelines say go lower-below 55 mg/dL if you’ve had a heart attack or have FH.
Step 4: Start treatment.
Statins are the first-line drug. Atorvastatin and rosuvastatin are the strongest. They can drop LDL by 50% or more. But about 1 in 5 people can’t tolerate them-muscle pain, fatigue, liver issues. If that’s you, ezetimibe is a good second option. It lowers LDL by 18%. It’s gentle. It’s cheap.
For those who need more, PCSK9 inhibitors (alirocumab, evolocumab) are injected every two weeks. They can knock off another 50-60% of LDL on top of statins. And now there’s inclisiran (Leqvio)-a shot only twice a year. It’s a game-changer for people who struggle with daily pills.
But here’s the problem: only about half of people who need statins actually take them after a year. And even fewer reach their target LDL. Why? Side effects. Cost. Forgetfulness. Lack of follow-up. That’s why regular check-ins with your doctor matter.
What About Diet and Lifestyle?
Yes, food matters. But not the way you think.
For years, we were told to avoid eggs and shellfish because they’re high in cholesterol. But the science changed. The 2020-2025 Dietary Guidelines removed the daily cholesterol limit. Why? Because for most people, dietary cholesterol doesn’t raise blood cholesterol much. Saturated fat does.
So focus here:
- Reduce saturated fat: cut back on butter, red meat, full-fat dairy, fried foods.
- Avoid trans fat: check labels for "partially hydrogenated oils."
- Eat more soluble fiber: oats, beans, lentils, apples, pears.
- Add plant sterols: found in fortified orange juice, margarines, and yogurt.
- Include nuts: almonds, walnuts, pistachios-1/4 cup a day.
- Choose fish: salmon, mackerel, sardines-omega-3s help lower triglycerides.
Exercise? At least 150 minutes a week of brisk walking. That’s 30 minutes, five days a week. It doesn’t have to be intense. Just consistent. It raises HDL (good cholesterol) and lowers triglycerides.
Weight loss? Losing just 5-10% of your body weight can drop LDL by 15%. That’s more than most pills.
Who’s at Risk?
It’s not just older men. Here’s who needs to be extra careful:
- Anyone with a family history of early heart disease (before age 55 in men, 65 in women)
- People with diabetes-68% have abnormal cholesterol
- Those with high blood pressure or obesity
- Smokers
- Women after menopause
- Black and Hispanic adults-statin use is significantly lower in these groups
And here’s the scary part: only 55.5% of U.S. adults who need statins are even getting them. Among Black adults, it’s 42.3%. Among women, 49.2%. That’s not just a gap in care-it’s a gap in survival.
What’s New in 2025?
Things are changing fast.
Inclisiran (Leqvio), approved in 2021, is now widely available. It’s a single shot twice a year that cuts LDL by half. No daily pills. No remembering. Just two visits a year.
Genetic testing is becoming more common. Polygenic risk scores can now tell you if your high cholesterol comes from dozens of small gene variations-not one big mutation. That helps doctors tailor treatment.
And new guidelines are pushing for earlier intervention. The International FH Foundation now recommends screening kids as young as 2 if a parent has FH. Why? Because plaques start forming in childhood.
But the biggest threat? Obesity. The CDC projects that by 2030, half of U.S. adults will be obese. That means more diabetes, more insulin resistance, more secondary hypercholesterolemia. We’re heading for a perfect storm.
What Should You Do Right Now?
If you’re reading this, you might be worried. Maybe you got your results back. Or maybe a loved one had a heart attack. Here’s what to do next:
- Get a lipid panel if you haven’t had one in the last five years. If you’re over 40, or have risk factors, get it now.
- If your LDL is over 160, ask your doctor: "Could this be familial?"
- If you’re on statins, don’t stop because of side effects-talk to your doctor about alternatives.
- Start small with diet: swap butter for olive oil. Eat oatmeal instead of sugary cereal. Add a handful of nuts to your snack.
- Walk every day. Even 10 minutes counts.
- Follow up. Cholesterol isn’t a one-time fix. It’s a lifelong habit.
High cholesterol doesn’t have to be a death sentence. But it won’t fix itself. You have to act. Not someday. Not when you’re 50. Now. Because the next plaque you build might be the one that ends your life.
Can high cholesterol be reversed without medication?
Yes, for many people with acquired hypercholesterolemia, lifestyle changes can lower LDL by 30% or more. The Portfolio Diet, regular exercise, weight loss, and quitting smoking are proven methods. But if your LDL is above 190 mg/dL, especially with a family history, medication is usually necessary. Genetics can’t be changed by diet alone.
Is familial hypercholesterolemia rare?
It’s not rare-it’s underdiagnosed. About 1 in 250 people have heterozygous familial hypercholesterolemia. That means over a million Americans have it, but less than 10% know. Many are diagnosed only after a heart attack. Screening family members is critical.
Do eggs raise cholesterol?
For most people, dietary cholesterol from eggs has little effect on blood cholesterol. What matters more is saturated fat-found in bacon, butter, and fried foods. One egg a day is fine for healthy people. But if you have FH or diabetes, limit yolks and focus on overall diet patterns.
What are the side effects of statins?
The most common side effect is muscle aches, reported by 7-29% of users. Liver enzyme changes are rare and usually mild. Serious side effects like rhabdomyolysis (muscle breakdown) happen in fewer than 1 in 10,000 people. If you have muscle pain, don’t quit-talk to your doctor. Alternatives like ezetimibe or lower-dose statins often help.
Can children have high cholesterol?
Yes. Children with familial hypercholesterolemia can have LDL levels over 200 mg/dL from birth. The American Academy of Pediatrics recommends screening between ages 9 and 11, and again at 17-21. Early detection and treatment can prevent heart disease decades later.
How often should I get my cholesterol checked?
Every 4-6 years for adults without risk factors. If you have high cholesterol, diabetes, high blood pressure, or a family history, get tested every year or as your doctor recommends. After starting medication, check levels after 4-12 weeks to see if it’s working.
Are natural supplements like red yeast rice effective?
Red yeast rice contains monacolin K, which is chemically identical to lovastatin, a prescription statin. It can lower LDL, but it’s unregulated-potency and contamination vary. Some products contain harmful toxins. It’s not a safe substitute for prescribed medication, especially for high-risk patients. Always talk to your doctor before using supplements.
What’s Next?
High cholesterol is one of the most preventable causes of death. But prevention requires action. It’s not about being perfect. It’s about being consistent. A walk. A swapped meal. A blood test. A pill taken on time. These small things add up.
If you have high cholesterol, you’re not alone. But you’re also not powerless. The tools to fix it exist. The science is clear. The question isn’t whether you can change it-it’s whether you will.

Ryan Airey
Let’s be real - most people don’t care until they’re lying in a hospital bed with a stent in their artery. This post is accurate but feels like shouting into a void. The system is broken. Doctors don’t have time. Patients don’t understand. Insurance won’t cover the tests until it’s too late. And don’t get me started on how Pharma markets statins like candy while ignoring the root causes - sugar, stress, and sleep deprivation. We’re treating symptoms like they’re the disease.
ASHISH TURAN
Good breakdown. In India, we see a lot of young people with high LDL because of fried snacks, refined flour, and zero movement. My cousin, 28, had LDL of 210 - no family history, just diet and sitting all day. Changed to oats, dal, walking 6km daily. In 6 months, down to 125. No meds. It’s possible. But people think ‘natural’ means ‘easy’.
Aidan McCord-Amasis
Statins = mandatory. 😎
Adam Dille
I used to think cholesterol was just a number until my dad had a stroke at 52. He was ‘healthy’ - ran 3x a week, ate ‘clean.’ Turns out he had FH. We all got tested. I’m on a low-dose statin now. Not because I’m lazy, but because my genes are lazy. This post nailed it - genetics aren’t a myth, they’re a reality. Thanks for sharing.
Katie Baker
I love how you mentioned the Portfolio Diet - I started adding flaxseed and walnuts to my morning yogurt and honestly, it’s become my favorite part of the day. Small changes, big impact. Also, walking after dinner with my dog? Best therapy. 🐶
Jonathan Dobey
Here’s the uncomfortable truth no one wants to admit: cholesterol isn’t the villain - it’s the messenger. Your body makes it because it needs it. The real issue? Inflammation. Processed foods. Endocrine disruptors. Glyphosate in our grains. The medical industrial complex has sold us a narrative: take a pill, forget the system. But if you want to know why your LDL is high, look at your environment, not your mirror. The system is rigged to keep you sick. And they profit from your ignorance.
John Foster
There’s a quiet horror in the fact that we’ve normalized silent death. We check our phones more often than our lipid panels. We binge Netflix while our arteries calcify. We treat cholesterol like a dieting problem, not a biological emergency. We’re conditioned to believe that if we don’t feel it, it doesn’t exist. But biology doesn’t care about your denial. Plaque doesn’t pause for your next vacation. It doesn’t wait for you to ‘get around to it.’ It builds. Slowly. Relentlessly. Until one day, your heart says, ‘Enough.’ And then it’s too late. The tragedy isn’t that people don’t know - it’s that they know and still do nothing. We’ve turned prevention into a moral failing. And that’s the real disease.
Ogonna Igbo
USA always act like they invented medicine. We in Nigeria have been eating natural foods for centuries - millet, bitter leaf, ogbono soup. No statins needed. Your fast food and sugar drinks are the problem. You think a pill fixes everything? You are blind. Our grandmothers didn’t have cholesterol tests. They had food. Real food. Not this lab-made junk you call breakfast. Stop blaming genetics. Blame your greed for convenience.
BABA SABKA
Let’s deconstruct the lipid panel mythos. LDL is not a toxin - it’s a repair molecule. It’s sent to sites of endothelial damage to patch microtears. The real issue is oxidative stress from polyunsaturated seed oils - canola, soybean, sunflower - which are literally in every processed food you eat. Statins reduce cholesterol but don’t address the root: lipid peroxidation. And PCSK9 inhibitors? They’re just Band-Aids on a hemorrhaging artery. The pharmaceutical model is designed to monetize chronicity, not cure it. We need to stop pathologizing physiology.
Hollis Hollywood
I read this whole thing while sitting in my car after my checkup. My LDL was 187. I’ve been avoiding meat and dairy for months, but I still eat a ton of cheese. I thought I was doing okay. This made me cry. Not because I’m scared - but because I realized I’ve been lying to myself. I don’t need a miracle. I need to stop eating cheese before bed. And maybe walk with my sister instead of scrolling. Thank you for writing this. It didn’t scare me. It just reminded me I’m still in control.
Edward Ward
One thing nobody talks about: the psychological toll of being told you’re ‘at risk’ when you feel fine. It creates a weird kind of hypochondria - you start checking your pulse, obsessing over every twinge, wondering if that headache is a stroke waiting to happen. I’ve been on a statin for three years. My LDL is 78. But I still feel like a ticking time bomb. The medical system gives you data, but rarely gives you peace. Maybe we need to stop treating cholesterol like a criminal and start treating it like a misunderstood neighbor who just needs a little help.
Chris Bryan
Who funded this? The pharmaceutical lobby? The CDC? The WHO? They’ve been pushing statins since the 90s while hiding the fact that 75% of heart attacks happen in people with ‘normal’ cholesterol. They’re selling fear. Cholesterol isn’t dangerous - it’s your body’s defense system. They want you dependent on pills so you’ll keep paying. And they’ve brainwashed you into thinking your body is broken. It’s not. It’s been poisoned by government dietary guidelines that told you to eat low-fat cereal and margarine. That’s the real epidemic.