One glass of grapefruit juice in the morning might seem harmless-maybe even healthy. But if you’re taking certain medications, that glass could be dangerous. It’s not just a myth or a warning you hear once and forget. This is a real, well-documented, and sometimes deadly interaction that affects more than 85 prescription drugs in the U.S. alone. And it doesn’t matter if you drink it once a week or every day. Even a single glass can change how your body handles your medicine-sometimes for up to three days.
Why Grapefruit Juice Interacts With Medications
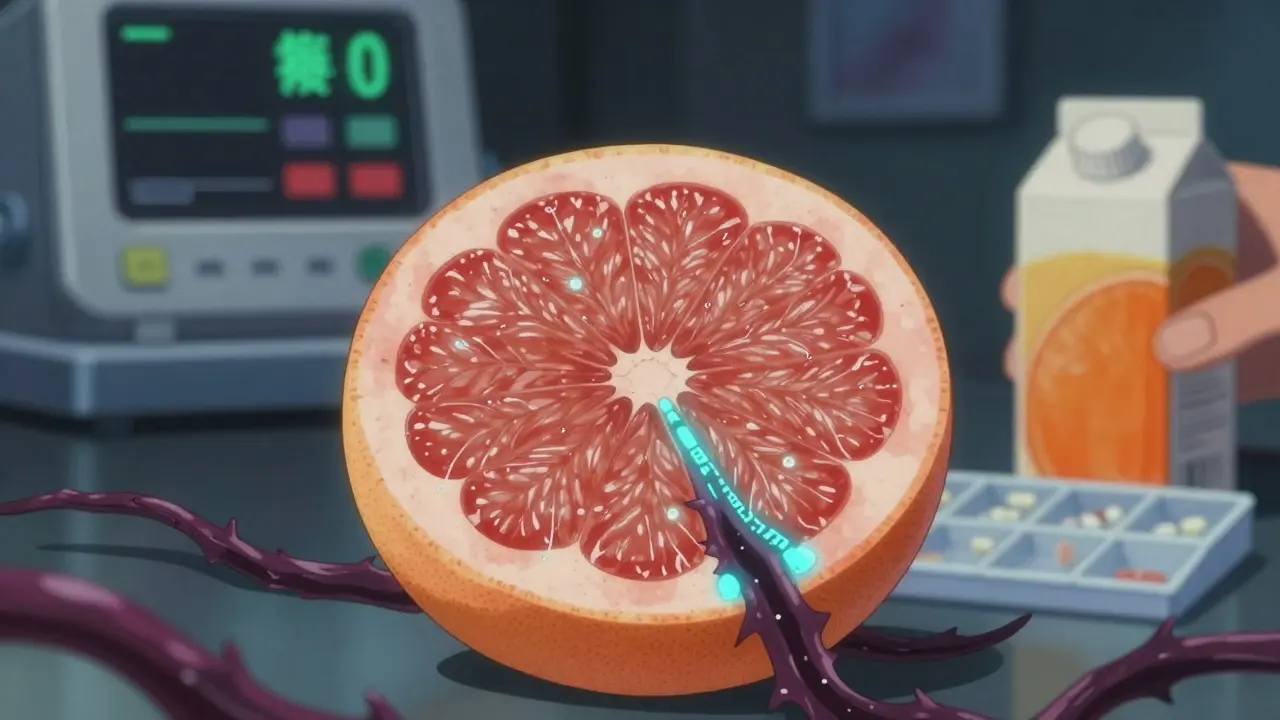
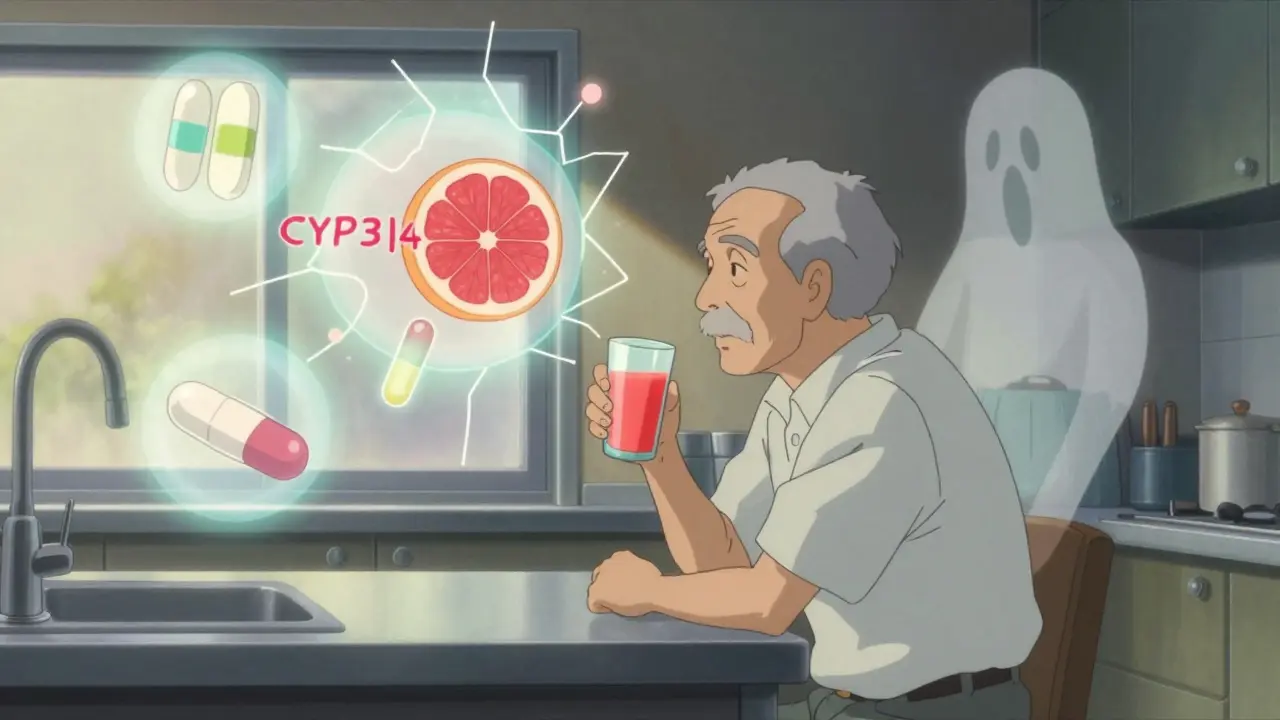
Grapefruit juice doesn’t just mix poorly with some pills-it actively changes how your body absorbs them. The culprit isn’t sugar or acid. It’s a group of natural chemicals called furanocoumarins, mainly bergamottin and 6',7'-dihydroxybergamottin. These compounds attack an enzyme in your gut called CYP3A4. This enzyme is like a gatekeeper. It normally breaks down a huge portion of oral medications before they enter your bloodstream. When grapefruit juice knocks out this enzyme, more of the drug slips through untouched.What happens next? Your blood ends up with way more of the drug than intended. That’s not a bonus-it’s a risk. Too much of a blood pressure pill can drop your pressure dangerously low. Too much of a cholesterol drug can wreck your muscles. Too much of a heart rhythm drug can trigger a fatal arrhythmia. And here’s the kicker: this effect lasts for days. One glass of juice can shut down CYP3A4 for 24 to 72 hours. So even if you take your pill at night and drink grapefruit juice in the morning, you’re still at risk.
Which Medications Are Most at Risk?
Not all drugs are affected equally. But some are especially dangerous when mixed with grapefruit. Here are the top categories and specific examples:- Statins (cholesterol drugs): Simvastatin (Zocor) is the worst offender. Just one glass of grapefruit juice can triple the amount of simvastatin in your blood, raising your risk of rhabdomyolysis-a condition where muscle tissue breaks down and can lead to kidney failure. Atorvastatin (Lipitor) has a milder interaction, but it’s still risky. Pravastatin and rosuvastatin? Safe. No interaction.
- Calcium channel blockers (blood pressure drugs): Felodipine (Plendil) sees a fivefold increase in blood levels. Nifedipine (Procardia) jumps by 3.3 times. Amlodipine (Norvasc)? No problem. The difference matters because some of these drugs are used to prevent heart attacks.
- Immunosuppressants: Cyclosporine (Neoral), used after organ transplants, can spike 50-60% in concentration. That’s enough to cause severe kidney damage.
- Antiarrhythmics: Amiodarone (Cordarone) levels rise 30-40%. For someone with a heart condition, this can mean sudden, life-threatening irregular rhythms.
- Other high-risk drugs: Some sedatives like midazolam, certain opioids like oxycodone, and even some psychiatric meds like quetiapine can become dangerously potent.
On the flip side, many common drugs show little to no interaction. Trazodone, zolpidem, and most antidepressants like sertraline are generally safe. But you can’t assume. Always check.
Not All Citrus Is the Same
If you love citrus and you’re on medication, you might be wondering: can I just switch to orange juice? The answer is… maybe. Sweet oranges (like navel or Valencia), lemons, and limes are safe. They don’t contain furanocoumarins. But Seville oranges-used in traditional marmalade-and pomelos? They’re just as dangerous as grapefruit. Same chemicals. Same risk.Even within grapefruit, not all varieties are equal. White grapefruit has higher levels of furanocoumarins than red or pink. Fresh-squeezed juice is stronger than store-bought pasteurized versions. And don’t think eating the fruit is safer. The peel and pulp contain the same compounds. It’s the juice, the pulp, the whole thing.

Who’s Most at Risk?
This isn’t just about what you’re taking-it’s about who you are. Older adults are especially vulnerable. People over 65 make up 40% of grapefruit juice drinkers in the U.S. and are also the ones most likely to be on five or more medications. That’s a dangerous combo.Also, your body’s natural CYP3A4 levels vary. Some people have more of the enzyme, some have less. That’s why two people taking the same drug and drinking the same amount of grapefruit juice can have wildly different outcomes. One might feel fine. The other ends up in the hospital. There’s no test to know your baseline. So the only safe rule? Avoid it completely if you’re on a risky medication.
What Should You Do?
You don’t need to guess. Here’s what actually works:- Check your prescription labels. Since 2014, the FDA has required manufacturers to include grapefruit warnings on affected drug labels. Look for phrases like “avoid grapefruit” or “do not consume grapefruit products.”
- Talk to your pharmacist. A 2021 study found that 89% of community pharmacists routinely screen for grapefruit interactions when filling prescriptions. Don’t assume they’ll bring it up-ask. Say: “Does this interact with grapefruit?”
- Keep a full medication list. Include every pill, patch, supplement, and over-the-counter drug. Some antihistamines like fexofenadine (Allegra) are affected. So are certain cough syrups and herbal products. Don’t leave anything out.
- Ask about alternatives. If you’re on simvastatin, your doctor might switch you to pravastatin or rosuvastatin. If you’re on cyclosporine, tacrolimus might be a safer option. These switches are common and effective.
- Don’t wait for symptoms. You won’t feel the interaction coming. Muscle pain, weakness, dizziness, irregular heartbeat, nausea-these can be signs of toxicity. But by the time you notice them, damage may already be done.
What About the Future?
Scientists are working on solutions. In October 2023, the USDA announced that CRISPR-edited grapefruit with 90% less furanocoumarin had passed early safety tests. That could mean a future where you can enjoy grapefruit without risk. But that’s years away. Right now, the only proven protection is avoidance.Drug makers have already lost over $1.2 billion in annual sales because patients stopped taking simvastatin to avoid grapefruit. That’s how serious this is. And yet, a 2022 survey found only 38% of patients remembered being warned about grapefruit when they got their prescription. That’s not just negligence-it’s a public health gap.
Bottom Line: When in Doubt, Skip It
Grapefruit juice isn’t evil. It’s full of vitamin C and antioxidants. But when it’s mixed with certain medications, it turns from a healthy drink into a hidden danger. The science is clear. The warnings are real. The consequences can be fatal.You don’t need to give up citrus forever. Just know which ones are safe and which ones aren’t. And if you’re on any medication-especially for cholesterol, blood pressure, heart rhythm, or after a transplant-ask your doctor or pharmacist: “Is grapefruit safe with this?” Don’t rely on memory. Don’t assume it’s okay. When the stakes are this high, caution isn’t overkill. It’s essential.
Can I drink grapefruit juice if I take my medication at a different time of day?
No. The enzyme-blocking effect of grapefruit juice lasts 24 to 72 hours. Even if you take your pill at night and drink juice in the morning, the enzyme is still inhibited. The timing doesn’t matter-only the presence of grapefruit in your system. Avoid it entirely during your treatment.
Is grapefruit juice interaction the same for everyone?
No. Some people naturally have more CYP3A4 enzyme in their gut than others, so they experience stronger interactions. But there’s no simple test to measure this. That’s why experts say the safest approach is to avoid grapefruit entirely if you’re on a medication known to interact with it.
What about grapefruit-flavored sodas or candy?
Most grapefruit-flavored sodas, candies, or extracts use artificial flavoring and do not contain furanocoumarins. But if the label says “real grapefruit juice” or lists grapefruit as an ingredient, treat it the same as fresh juice. Always check the ingredient list.
Can I eat the whole grapefruit instead of drinking the juice?
No. The furanocoumarins are in the pulp, peel, and juice. Eating the fruit delivers the same risk as drinking the juice. The form doesn’t matter-the chemicals do.
Are there any medications that are safe with grapefruit?
Yes. Many drugs, including sertraline, citalopram, levothyroxine, and metformin, have no known interaction with grapefruit. But you can’t assume. Always verify with your doctor or pharmacist. The list of safe drugs changes as new research comes out.
Roshan Gudhe
Man, I never realized grapefruit juice could mess with my meds like that. I’ve been drinking it every morning with my statin, thinking it was just a healthy habit. Guess I’m switching to orange juice now. 🍊
Rachel Kipps
i didnt know this was a thing. my dr never mentioned it. i guess i should call them. thanks for the heads up.
Prajwal Manjunath Shanthappa
Let’s be clear: this isn’t ‘a risk’-it’s a biochemical betrayal. The pharmaceutical industry has known about CYP3A4 inhibition since the 1990s, yet patients are still being left in the dark? This isn’t negligence-it’s systemic malfeasance. And don’t even get me started on how the FDA’s labeling requirements are laughably inadequate. A single asterisk? Please. This deserves a full-page, neon-red warning in every prescription bottle. The fact that 62% of patients remain unaware is a moral failure.
Wendy Lamb
Switched to orange juice after my pharmacist flagged it. So simple, but so important.
Antwonette Robinson
Wow. So the government requires a warning label, but your doctor? Nope. Not their job. And your pharmacist? Only if you ask. And you’re supposed to remember to ask? This isn’t healthcare-it’s a scavenger hunt for survival.
Jhoantan Moreira
This is such an important post. I’ve got an aunt on cyclosporine after her transplant, and she loved her morning grapefruit. Now she’s switched to apples. Small change, big difference. Thanks for sharing the science clearly.
Shelby Price
So… grapefruit-flavored soda is fine? Just not the real juice? I’ve been drinking that since college. Phew.
Nathan King
It is noteworthy that the furanocoumarin content varies significantly among cultivars and processing methods. One must exercise rigorous diligence in distinguishing between commercial juice products and freshly extracted equivalents, as the latter exhibits markedly higher inhibitory potency. Furthermore, the temporal persistence of CYP3A4 suppression underscores the necessity of complete abstinence, rather than temporal separation.
Demetria Morris
People who drink grapefruit juice while on meds are just asking for trouble. You think you’re being healthy, but you’re just being reckless. Your body isn’t a lab experiment.
Geri Rogers
THIS IS SO IMPORTANT. I’m a pharmacist and I see this every day. People say, ‘But I only drink it once a week!’ - and I have to explain it’s not about frequency, it’s about the enzyme shutdown. I keep printed handouts on my counter. Please, if you’re on meds, ask. Don’t assume. I’ve seen people end up in the ER over this. Don’t be one of them. 💪
Samuel Bradway
My grandpa’s on blood pressure meds. I’m gonna print this out and leave it on his fridge. He thinks ‘natural’ means safe. Nope.
Caleb Sutton
Big Pharma doesn’t want you to know this. They profit off the side effects. They’ve been suppressing research on safe citrus alternatives for decades. This is why you can’t trust the system.
Janice Williams
It is deeply regrettable that laypersons continue to confuse culinary preference with pharmacological prudence. The conflation of ‘natural’ with ‘benign’ is not merely erroneous-it is a dangerous intellectual failing. One does not, after all, consume arsenic because it is ‘mineral-rich.’
Alex LaVey
Love that this post includes the CRISPR update. Science is moving fast. Maybe one day we’ll have safe grapefruit. Until then, orange juice it is. 🍊
caroline hernandez
From a clinical pharmacology standpoint, the pharmacokinetic variability of CYP3A4 expression across the gut epithelium is a key confounder. Genotypic polymorphisms (e.g., CYP3A5*3) further modulate this interaction. Therefore, personalized risk stratification is imperative-but since that’s not scalable, population-level avoidance remains the most effective harm-reduction strategy.