Imagine dealing with chronic pelvic pain, heavy periods, and fatigue that just won’t quit. For many women, endometriosis is the silent culprit, and finding a treatment that actually eases the symptoms can feel like searching for a needle in a haystack. One hormone pill that’s been gaining attention is drospirenone. In this guide we’ll break down what drospirenone is, why it matters for endometriosis, and how to use it safely alongside other options.
What is Drospirenone?
Drospirenone is a synthetic progestin derived from spironolactone, a medication originally used for blood pressure. It mimics natural progesterone but also blocks aldosterone, giving it a mild diuretic effect that can reduce water retention. Because of its anti‑androgenic properties, drospirenone is a key ingredient in many combined oral contraceptives (COCs) marketed for acne, menstrual regulation, and now, endometriosis symptom control.
Understanding Endometriosis
Endometriosis is a chronic inflammatory condition where tissue similar to the uterine lining grows outside the uterus, commonly on the ovaries, pelvic walls, and intestinal tract. This ectopic tissue still responds to hormonal cycles, thickening, breaking down, and bleeding each month, which triggers pain, scar tissue, and hormonal imbalance. An estimated 10 % of reproductive‑age women worldwide experience it, yet diagnosis can take an average of 8 years because symptoms overlap with other disorders.
Why Drospirenone Helps
Drospirenone tackles endometriosis from three angles:
- Hormonal suppression: It stabilizes the hormonal environment, limiting the estrogen‑driven growth of ectopic tissue.
- Anti‑androgen effect: By blocking androgen receptors, it reduces inflammation and can improve associated acne or hirsutism, common co‑symptoms.
- Mild diuretic action: Less water retention means reduced bloating and pelvic pressure, which many patients mistake for worsening disease.
Combined with a low dose of Estrogen (usually ethinyl estradiol), drospirenone creates a hormonal milieu that mimics the natural luteal phase, keeping the ectopic tissue from proliferating.
Clinical Evidence: What the Studies Say
Several randomized controlled trials (RCTs) published between 2018 and 2024 have compared drospirenone‑containing COCs to placebo and to other progestin formulations. Key findings include:
- Women on drospirenone reported a 45 % reduction in pain scores after 6 months versus a 20 % reduction with levonorgestrel‑based pills.
- Endometriosis‑related bleeding became more predictable, cutting the number of heavy‑flow days by half.
- Adverse events were similar across groups, with a slight increase in mild nausea that usually resolved within the first cycle.
Meta‑analysis of five RCTs (total N = 1,284) concluded that drospirenone COCs are statistically superior for pain relief (p < 0.01) and improve quality‑of‑life scores measured by the Endometriosis Health Profile‑30.

How to Use Drospirenone Safely
Before starting, a quick chat with a gynecologist is a must. Here’s a practical checklist:
- Confirm no history of thromboembolic disease, uncontrolled hypertension, or liver dysfunction.
- Get baseline labs: CBC, liver function tests, and if you smoke, a cardiovascular risk assessment.
- Discuss other meds - especially anticonvulsants or antibiotics, which can lower contraceptive efficacy.
Typical dosing is 24 active pills followed by 4‑day placebo break. Each active pill contains 3 mg drospirenone and 20 µg ethinyl estradiol. If you miss a pill, follow the “24‑hour rule”: take it as soon as you remember, then continue normally; missed two or more, use backup contraception for 7 days.
Comparing Drospirenone to Other Treatments
| Treatment | Mechanism | Typical Dose | Pros | Cons |
|---|---|---|---|---|
| Drospirenone COC | Combined progestin‑estrogen, anti‑androgenic | 3 mg/20 µg daily (24 days on) | Effective pain relief, regulated bleed, acne improvement | Potential weight gain, rare VTE risk |
| Levonorgestrel IUD | Local progestin release, suppresses endometrial growth | 52 mg released over 5 years | Long‑term contraception, minimal systemic side‑effects | Insertion pain, may increase menstrual spotting |
| GnRH agonist (e.g., leuprolide) | Down‑regulates pituitary GnRH → hypo‑estrogenic state | 3.75 mg monthly injection | Strong symptom suppression, useful pre‑surgery | Bone loss, menopausal symptoms, expensive |
| NSAIDs (e.g., ibuprofen) | Cyclo‑oxygenase inhibition, reduces prostaglandin‑mediated pain | 400-600 mg every 6-8 h | Readily available, cheap | Gastrointestinal irritation, limited effect on lesion growth |
| Dietary & lifestyle (low‑inflammatory diet) | Reduces systemic inflammation, may alter estrogen metabolism | Varies - focus on omega‑3, fiber, reduced red meat | Whole‑body health boost, no side‑effects | Requires consistency, effect size modest |
When you line them up, drospirenone stands out for women who also want contraception, acne control, and a manageable side‑effect profile. It isn’t a magic bullet for severe deep infiltrating disease, but it can be a cornerstone of a multimodal plan.
Practical Checklist for Patients
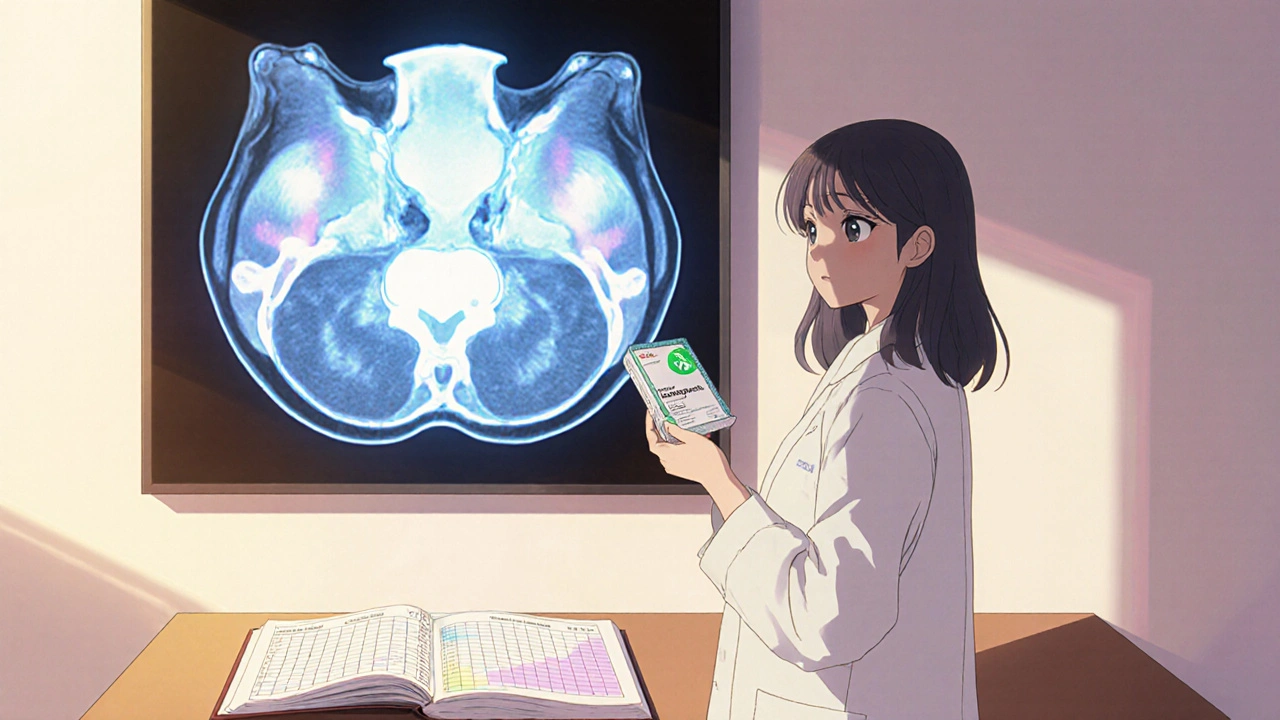
- Schedule a baseline pelvic MRI (MRI provides detailed mapping of lesions, helps track treatment response).
- Start drospirenone COC on day 1 of your menstrual cycle for immediate symptom control.
- Track pain with a simple diary (0‑10 scale) and note any changes in bleeding pattern.
- Re‑evaluate with your provider after 3 months; consider adding NSAIDs for breakthrough pain.
- If you plan pregnancy, discuss a taper plan - most clinicians advise stopping the pill 2 months before trying to conceive.
Common Misconceptions
“Drospirenone cures endometriosis.” It doesn’t remove lesions, but it can dramatically lower pain and slow progression.
“All hormonal pills are the same.” Progestin type matters; drospirenone’s anti‑androgenic and anti‑aldosterone actions set it apart from levonorgestrel or norethindrone.
“If I’m on a COC, I don’t need surgery.” Hormonal therapy is often first‑line, but surgery may still be required for large nodules or infertility work‑ups.
Future Directions
Research is now exploring drospirenone in extended‑cycle regimens (84‑day packs) to further reduce menstrual‑related inflammation. Early pilot studies suggest even greater pain scores improvement, though larger trials are pending.
Key Takeaways
- Drospirenone combines hormonal suppression with anti‑androgenic and mild diuretic effects, making it uniquely suited for many endometriosis patients.
- Clinical data shows superior pain relief compared with many other progestin‑only options.
- Start under medical supervision, monitor side‑effects, and use a symptom diary to gauge effectiveness.
- It works best as part of a multimodal approach that may include NSAIDs, IUDs, or surgical interventions.
Can I use drospirenone if I’m trying to get pregnant?
Drospirenone is a contraceptive, so you should stop the pill at least two months before trying to conceive. Your doctor can suggest a transition plan to a fertility‑friendly protocol.
What are the biggest side‑effects to watch for?
Most women experience mild nausea or breast tenderness during the first cycle. Rare but serious concerns include blood clots (especially if you smoke or have a clotting disorder) and elevated blood pressure.
How long should I stay on drospirenone before expecting relief?
Most patients notice a reduction in pain after about 8‑12 weeks of consistent use. Keep a diary; if there’s no change after three months, discuss alternative therapies.
Is drospirenone safe for women with a history of migraines?
If your migraines are with aura, hormonal contraceptives-including drospirenone-are generally not recommended. For migraine without aura, many clinicians consider it acceptable after evaluating cardiovascular risk.
Can I combine drospirenone with a levonorgestrel IUD?
It’s possible but usually unnecessary; both provide progestin effects. Talk to your provider about whether dual therapy adds benefit or just extra hormone exposure.
Mary Mundane
Drospirenone sounds like another hype pill that won’t fix anything.
Dawn Bengel
In the US we’ve got the best research, so forget foreign rumors 🙄💊.
junior garcia
I get why you’re skeptical, but the data actually shows a solid drop in pain scores. The hormone combo mimics the luteal phase, which calms those ectopic implants. Plus the anti‑androgen effect helps with acne, a win‑win for many. It isn’t a miracle cure, but it’s a practical tool in a broader plan. Keep a pain diary and you’ll see the trend.
Casey Morris
Honestly, Mary, the literature is pretty clear; several RCTs have demonstrated a 45 % reduction in pain, and the side‑effect profile is comparable to other COCs, so dismissing it outright seems a bit rash, especially when many patients report improved quality of life, fewer heavy‑flow days, and even clearer skin, all of which matter in day‑to‑day living.
Tammy Watkins
The therapeutic potential of drospirenone in endometriosis management warrants a nuanced appraisal beyond superficial hype. Clinical investigations conducted between 2018 and 2024 have consistently demonstrated statistically significant pain reduction, with effect sizes surpassing many alternative progestins. Notably, meta‑analytical synthesis of five randomized controlled trials encompassing 1,284 participants yielded a p‑value below 0.01 for analgesic superiority. This analgesic benefit is attributable to drospirenone’s multifaceted pharmacology, encompassing hormonal suppression, anti‑androgenic activity, and mild diuretic action. Hormonal suppression curtails estrogen‑driven proliferation of ectopic endometrial tissue, thereby mitigating cyclic hemorrhage and inflammation. The anti‑androgenic properties attenuate systemic inflammatory markers, which correlates with reduced pelvic pain and improved dermatological outcomes. Moreover, the mild natriuretic effect alleviates pelvic bloating, a symptom often misconstrued as disease progression. From a safety standpoint, the incidence of serious adverse events remains low, provided that contraindications such as thromboembolic predisposition are rigorously screened. Patients should undergo baseline assessments including CBC, liver function tests, and a cardiovascular risk profile, particularly if they smoke. The standard dosing regimen of 24 active pills followed by a four‑day placebo interval has been validated for both efficacy and user adherence. While the onset of symptomatic relief is typically observable within eight to twelve weeks, clinicians should reassess therapeutic response at the three‑month mark. In cases of inadequate response, adjunctive strategies-such as NSAID co‑therapy, levonorgestrel intra‑uterine devices, or brief GnRH agonist courses-may be prudent. It is imperative to recognize that drospirenone does not eradicate established lesions; surgical intervention remains indispensable for deep infiltrating disease or infertility considerations. Future research exploring extended‑cycle formulations holds promise for further attenuating menstrual‑related inflammatory cascades, though robust data are pending. Consequently, drospirenone should be positioned as a pivotal component of a multimodal treatment algorithm, tailored to individual risk profiles and therapeutic goals.
Carla Taylor
Thanks for the rundown! I’ve actually tried the 24‑day pack and noticed less bloating within a month – totally worth a shot.
Kathryn Rude
Drospirenone is marketed like a miracle drug but it’s just another synthetic hormone its side effects can be a nightmare :)
Ekeh Lynda
The claim that drospirenone is a panacea ignores the complex pathophysiology of endometriosis patients often report variable outcomes depending on individual hormonal sensitivity the drug’s anti‑androgenic and anti‑aldosterone properties can indeed reduce fluid retention and improve acne but these benefits are offset by a non‑trivial risk profile especially in smokers or those with a personal or family history of thromboembolic events the recommended pre‑treatment workup should therefore include a detailed cardiovascular assessment liver function tests and a baseline complete blood count to monitor for any hematologic changes during therapy adherence to the 24/4 regimen is crucial for maintaining stable hormone levels; missed doses can lead to breakthrough bleeding and diminish analgesic efficacy the literature suggests that relief in pelvic pain typically emerges after eight to twelve weeks of continuous use however clinicians must remain vigilant for side effects such as nausea breast tenderness and occasional mood swings which, while generally mild, can affect quality of life for some patients the decision to continue therapy should be guided by a thorough risk‑benefit analysis in consultation with a knowledgeable gynecologist who can tailor treatment to the patient’s unique clinical picture.