Antibiotic Cost Comparison Tool
This tool compares generic antibiotic costs for a typical 10-day course. Costs may vary based on location, insurance, and pharmacy. Always consult your healthcare provider for the appropriate medication for your condition.
| Antibiotic | Cost Range | Dosing Frequency | Common Use Cases | Key Considerations |
|---|---|---|---|---|
| Amoxicillin | $5-$10 | 2-3 times/day | Strep throat, ear infections | First-line for many infections; not effective against resistant bacteria |
| Augmentin (amoxicillin/clavulanate) | $15-$40 | 2-3 times/day | Resistant sinus, skin, ear infections | Effective against beta-lactamase-producing bacteria; higher stomach side effects |
| Cephalexin | $10-$25 | 3-4 times/day | Skin infections, urinary tract | Good option for penicillin allergies; not effective against resistant bacteria |
| Doxycycline | $10-$20 | 1-2 times/day | Sinus, Lyme, acne, respiratory | Convenient dosing; can cause sun sensitivity |
| Azithromycin | $15-$30 | 1 time/day | Sinus, bronchitis, ear infections | Shortest course (3-5 days); not for deep skin infections |
| Clindamycin | $20-$50 | 3-4 times/day | Deep skin infections, abscesses | High risk of C. diff infection; use only when necessary |
When your doctor prescribes Augmentin, you’re getting a one-two punch against stubborn infections. It’s not just amoxicillin - it’s amoxicillin plus clavulanate, a combo designed to beat bacteria that laugh at regular penicillin. But what if Augmentin doesn’t work for you? Or maybe you had a rash, or it gave you stomach cramps, or your insurance won’t cover it? You’re not alone. Many people end up asking: what else can I take instead?
What Makes Augmentin Different
Augmentin is a brand name for a mix of two drugs: amoxicillin and a beta-lactamase inhibitor called clavulanate. Amoxicillin is a common penicillin-type antibiotic that kills bacteria by breaking down their cell walls. But some bacteria fight back by producing an enzyme called beta-lactamase that destroys amoxicillin before it can work.
That’s where clavulanate comes in. It doesn’t kill bacteria itself. Instead, it blocks the enzyme that bacteria use to neutralize amoxicillin. Think of it like a bodyguard for amoxicillin - it takes out the enemy’s weapon so amoxicillin can do its job. This combo makes Augmentin effective against infections that amoxicillin alone can’t touch, like sinus infections caused by resistant strains, certain ear infections, skin abscesses, and some types of pneumonia.
It’s not a first-line choice for every infection. Doctors usually start with plain amoxicillin for simple cases like strep throat or mild ear infections. Augmentin steps in when those fail, or when the infection looks like it’s coming from bacteria known to resist standard penicillin.
Common Alternatives to Augmentin
If Augmentin isn’t right for you, here are the most commonly prescribed alternatives - each with its own strengths and limits.
- Cephalexin - A first-generation cephalosporin, often used for skin and soft tissue infections. It’s a good substitute if you’re allergic to penicillin but not to cephalosporins. It doesn’t have a clavulanate partner, so it won’t work against beta-lactamase-producing bacteria. But for many common infections, it’s just as effective as Augmentin.
- Doxycycline - A tetracycline antibiotic that works differently than penicillins. It’s often used for respiratory infections, acne, Lyme disease, and some sinus infections. It’s not a direct replacement for Augmentin, but it’s effective against many of the same bacteria, especially if they’re resistant to penicillin. It’s also taken once or twice a day, which some people find easier than Augmentin’s three-times-daily dosing.
- Azithromycin - A macrolide antibiotic, often called a Z-Pack. It’s used for bronchitis, sinus infections, and some ear infections. It’s taken once a day for just 3-5 days, which makes it more convenient. But it’s not as broad-spectrum as Augmentin and doesn’t cover all the same bugs. It’s also not ideal for skin infections with pus.
- Clindamycin - Often used for skin and soft tissue infections, especially abscesses. It’s a strong choice if you’re allergic to penicillin and cephalosporins. It’s also effective against anaerobic bacteria - the kind that thrive in low-oxygen environments like deep wounds or dental infections. But it carries a higher risk of causing severe diarrhea from C. difficile, so it’s not usually a first pick unless necessary.
- Ciprofloxacin - A fluoroquinolone used for more serious infections like urinary tract infections, kidney infections, or certain types of pneumonia. It’s powerful, but not used lightly. The FDA warns against using fluoroquinolones for simple infections because of rare but serious side effects like tendon rupture and nerve damage. It’s not a direct substitute for Augmentin in most cases.
When to Choose One Over the Other
Choosing the right alternative isn’t about picking the strongest antibiotic - it’s about matching the drug to the infection, your medical history, and your body’s reaction to meds.
If you had a mild rash on Augmentin, you might still tolerate plain amoxicillin. But if you had a true allergic reaction - swelling, trouble breathing, hives - you need to avoid all penicillin-related drugs. In that case, doxycycline, azithromycin, or clindamycin become the go-to options.
For a sinus infection that didn’t clear up after 7 days on amoxicillin, Augmentin is the logical next step. If Augmentin didn’t work, doxycycline or a nasal steroid might be added. But if you’re still sick after two rounds of antibiotics, you might need a culture - meaning a sample of the infection is tested to find out exactly what’s causing it.
For a skin abscess, clindamycin or cephalexin are often preferred over Augmentin because they penetrate pus better. For a urinary tract infection, ciprofloxacin or nitrofurantoin are more targeted. Augmentin isn’t wrong here - it just isn’t the best fit.
Age matters too. Azithromycin is often used in kids because it’s easier to swallow and comes in flavored liquid. Doxycycline isn’t given to children under 8 because it can stain developing teeth. Clindamycin is avoided in older adults unless necessary because of the high risk of C. diff.
Side Effects and Tolerability
Augmentin is known for causing stomach upset. About 1 in 10 people get diarrhea, nausea, or vomiting. Some get yeast infections. The clavulanate part is usually the culprit - plain amoxicillin is much gentler on the gut.
Compare that to doxycycline: it can make you sensitive to sunlight and causes heartburn if taken on an empty stomach. Azithromycin is easier on the stomach but can cause temporary heart rhythm changes in people with existing heart conditions. Clindamycin carries a 5-10% risk of C. diff infection - a serious, sometimes life-threatening diarrhea that needs special antibiotics to treat.
That’s why many people switch from Augmentin not because it didn’t work, but because they couldn’t tolerate it. If you had bad side effects, your doctor might try a lower dose, switch to a different formulation (like a chewable or liquid), or pick a completely different class of antibiotic.
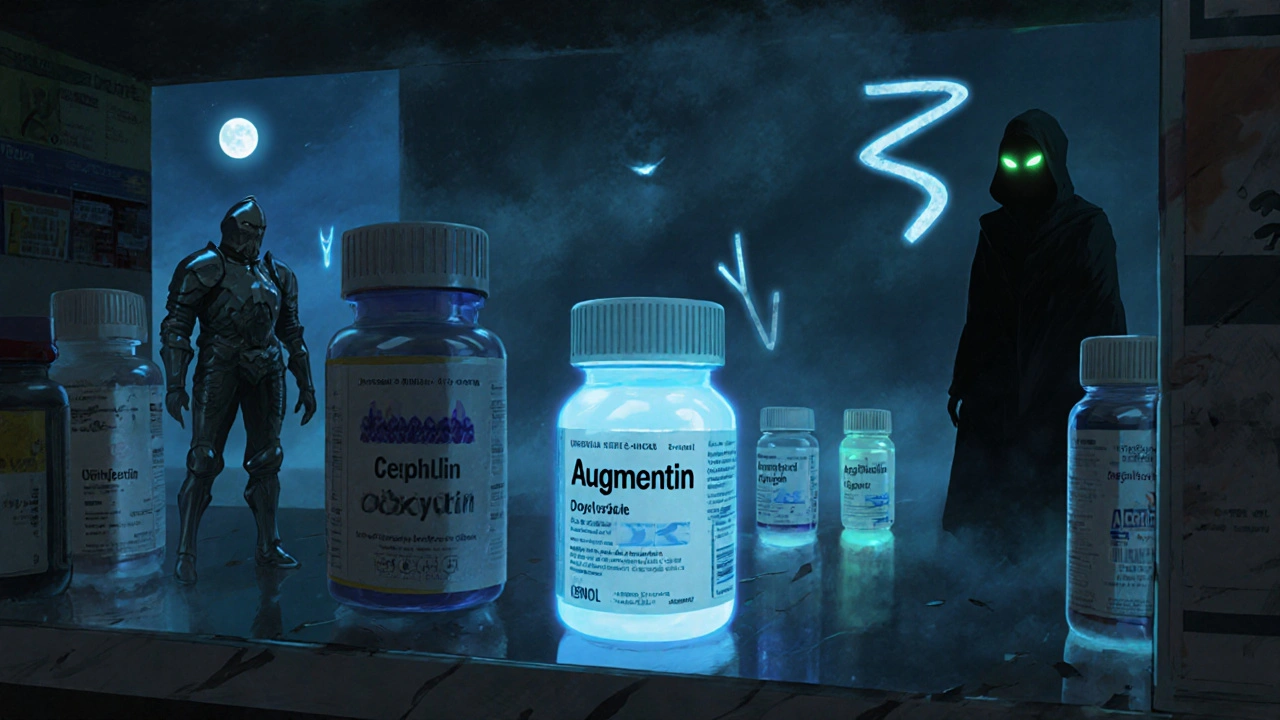
Cost and Accessibility
Augmentin isn’t cheap. The brand version can cost over $100 without insurance. But generic amoxicillin/clavulanate is widely available and usually under $20 for a 10-day course. That’s still more than plain amoxicillin, which can be as low as $5.
Here’s how the alternatives stack up in cost (for a typical 10-day course, generic versions):
| Antibiotic | Typical Cost (USD) | Frequency per Day | Common Use Cases |
|---|---|---|---|
| Amoxicillin | $5-$10 | 2-3 | Strep throat, ear infections |
| Augmentin (amoxicillin/clavulanate) | $15-$40 | 2-3 | Resistant sinus, skin, ear infections |
| Cephalexin | $10-$25 | 3-4 | Skin infections, urinary tract |
| Doxycycline | $10-$20 | 1-2 | Sinus, Lyme, acne, respiratory |
| Azithromycin | $15-$30 | 1 | Sinus, bronchitis, ear infections |
| Clindamycin | $20-$50 | 3-4 | Deep skin infections, abscesses |
Cost isn’t the only factor. Azithromycin’s five-day course is more convenient than Augmentin’s 10-day, three-times-a-day schedule. If you’re a busy parent or work long hours, fewer doses can mean better adherence - which means the infection is more likely to clear up.

What Doesn’t Work as an Alternative
Not every antibiotic you’ve heard of is a good substitute. Avoid these common misconceptions:
- Amoxicillin alone - If your infection is resistant to amoxicillin, adding clavulanate (Augmentin) was the right move. Going back to plain amoxicillin won’t help.
- Over-the-counter antibiotics - There are no FDA-approved oral antibiotics you can buy without a prescription in the U.S. Any website selling them is breaking the law and risking your health.
- Herbal supplements like garlic, echinacea, or oregano oil - These may support your immune system, but they don’t kill bacteria the way antibiotics do. Don’t use them to replace a prescribed course.
- Old leftover antibiotics - Taking an old prescription for a new infection is dangerous. The wrong drug, wrong dose, or expired med can make the infection worse or cause resistance.
What to Do If Augmentin Didn’t Work
If you finished your Augmentin course and you’re still sick - fever, pain, swelling - don’t just wait it out. Call your doctor. You might need:
- A different antibiotic - maybe one from a different class, like doxycycline or clindamycin.
- A culture - a swab or fluid sample tested in a lab to identify the exact bacteria and what kills it.
- An imaging test - like a sinus CT scan or ultrasound - to check for an abscess or other complication.
- A specialist referral - to an ENT, infectious disease doctor, or dermatologist, depending on the infection site.
Antibiotic resistance is real. Using the wrong drug or not finishing a course can make future infections harder to treat. That’s why switching antibiotics isn’t something to do on your own.
Final Thoughts
Augmentin is a powerful tool, but it’s not the only one. The best alternative depends on your infection, your history, your tolerance, and your life. Sometimes it’s cephalexin. Sometimes it’s doxycycline. Sometimes it’s just waiting and trying plain amoxicillin again.
The key is working with your doctor, not guessing. Antibiotics are powerful, but they’re not interchangeable. What works for one person’s ear infection might not work for your skin abscess. The right choice isn’t about what’s cheapest or easiest - it’s about what’s right for you.
Can I take amoxicillin instead of Augmentin?
Only if your infection is caused by bacteria that don’t produce beta-lactamase. If Augmentin was prescribed because plain amoxicillin didn’t work, switching back won’t help. Amoxicillin alone won’t kill resistant strains. Always check with your doctor before switching.
Is Augmentin stronger than amoxicillin?
Yes, but only against certain bacteria. Augmentin works against more types of infections because clavulanate blocks the enzyme that makes amoxicillin ineffective. For simple infections, amoxicillin is just as effective - and easier on your stomach. Augmentin isn’t stronger overall - it’s more targeted.
What’s the best alternative if I’m allergic to penicillin?
If you have a true penicillin allergy (hives, swelling, breathing trouble), avoid all penicillin-based drugs, including Augmentin. Safe alternatives include doxycycline, azithromycin, or clindamycin. Cephalexin is sometimes used if your allergy is mild, but only under doctor supervision. Never guess - get tested if you’re unsure.
Can I take Augmentin and azithromycin together?
Sometimes, yes - but only under medical supervision. Doctors may combine antibiotics for severe or complex infections, like pneumonia with multiple bacterial causes. But combining them without a reason increases side effects and risk of resistance. Never mix antibiotics on your own.
Why does Augmentin cause diarrhea?
The clavulanate part disrupts the balance of good bacteria in your gut. This can lead to mild diarrhea in about 10% of users. In rare cases, it can trigger a serious infection called C. diff. Taking probiotics may help, but if diarrhea is severe or bloody, stop the medication and call your doctor immediately.
How long does it take for Augmentin to work?
Most people start feeling better in 2-3 days. But you must finish the full course - even if you feel fine. Stopping early can leave behind the toughest bacteria, which then multiply and cause a worse infection later. If you don’t improve after 3 days, contact your doctor.
If you’ve been prescribed Augmentin and are wondering whether there’s a better option, you’re asking the right question. But the answer isn’t online - it’s in your medical history, your symptoms, and your doctor’s judgment. Don’t switch meds on your own. Talk to your provider. They’ll help you find the right fit - not just any alternative, but the one that works for you.
Sherri Naslund
lol so Augmentin is just amoxicillin with a bodyguard? what next, antibiotics with a personal trainer? i swear if i had a dollar for every time pharma made a drug sound like a superhero movie i could buy my own pharmacy. clavulanate? more like clavu-lame. why not just call it amoxicillin 2.0? 🤡
Lauren Hale
I’ve had patients switch from Augmentin to cephalexin after a rash, and honestly? It worked just fine for their cellulitis. The key is matching the bug, not just the brand. I’ve also seen folks on doxycycline for sinus infections who did way better than on Augmentin-less stomach drama, once-daily dosing. It’s not about strength, it’s about fit. And yeah, cost matters. A $5 amoxicillin script that works is better than a $40 one that makes you miserable. Trust your doc, but ask questions. You’re not just a name on a chart.
Donald Sanchez
bro i took augmentin last year for a tooth abscess and it made me feel like i swallowed a bag of angry hornets. diarrhea for 3 days straight 😭 then i switched to clindamycin and boom-felt better in 24h. but then my friend said clindamycin gives you C. diff like 1 in 10 times??? so now i’m scared to take ANYTHING. also why is doxycycline so cheap?? is the government subsidizing it or is big pharma just lazy?? 🤔
Ashley Miller
Funny how they never mention the real reason Augmentin exists: to keep you coming back for more. Clavulanate? More like a corporate patent loophole. They took a $0.05 generic and slapped on a $30 markup. Meanwhile, your doctor’s 'evidence-based' choice? Probably paid for by a rep with free lunch. And don’t get me started on 'culture tests'-that’s just a fancy way of saying 'we don’t know what we’re doing, so let’s send it to a lab and charge you $500.'
Greg Knight
Hey, if you’re reading this because you’re worried about your antibiotic options, you’re already ahead of the game. Most people just pop pills and hope. But you’re asking questions-that’s huge. I’ve seen too many folks quit antibiotics early because they 'felt better,' then end up back in the ER. Don’t do that. And if you had side effects? Tell your doc. Don’t just suffer silently. There’s almost always another option. Even if it’s not glamorous, like plain amoxicillin-it’s still effective. You’re not weak for needing help. You’re smart for seeking it.
rachna jafri
In India, we don’t even need a prescription for antibiotics. You walk into a pharmacy, say 'fever,' and they hand you ciprofloxacin like it’s candy. And guess what? People get better. But then they get resistant. And now the superbugs are here. Western doctors overthink everything-'culture this, test that, avoid this class.' Meanwhile, in rural UP, a 70-year-old grandma cures her son’s pneumonia with a single dose of azithromycin bought from a roadside stall. Who’s right? Maybe neither. But the system is broken. We need access, not algorithms.
darnell hunter
The structural integrity of the antibiotic classification system remains fundamentally compromised by the commercialization of beta-lactamase inhibitors. While the pharmacokinetic profile of amoxicillin-clavulanate demonstrates marginal efficacy against certain gram-negative organisms, the cost-benefit ratio is increasingly untenable given the availability of lower-risk alternatives such as doxycycline and cephalexin. Furthermore, the propensity for gastrointestinal adverse events renders Augmentin suboptimal for non-severe infections. A more rigorous, evidence-based protocol should prioritize narrow-spectrum agents prior to combination therapy.
Hannah Machiorlete
i took augmentin and it felt like my insides were being eaten by ants. i cried in the shower. then i went to the ER because i thought i was dying. turns out it was just diarrhea. now i’m terrified of every antibiotic. why do they even make these things? what if the next one gives me nerve damage? what if i wake up one day and my tendons just snap? i’m never taking another pill again. ever.
Bette Rivas
For community-acquired pneumonia, Augmentin is often appropriate if the patient has risk factors like recent antibiotic use or COPD. But for otherwise healthy adults with mild pneumonia, doxycycline or macrolides are preferred per IDSA guidelines. The key is local resistance patterns-what works in Chicago may not work in Miami. Also, clindamycin is excellent for skin abscesses, but only if you’re not over 65 or on PPIs. C. diff risk spikes dramatically with proton pump inhibitors. Always check drug interactions. And yes, probiotics help, but not all are equal-look for strains like Saccharomyces boulardii, not just 'digestive support' on the label.
prasad gali
The empirical prescribing paradigm of Augmentin reflects a systemic failure in antimicrobial stewardship. Clinicians default to broad-spectrum agents due to cognitive biases and time constraints, rather than microbiological diagnostics. The proliferation of beta-lactamase inhibitors is a pharmacoeconomic artifact, not a clinical imperative. Cephalexin, when appropriately selected, provides non-inferior outcomes in soft tissue infections with reduced selective pressure. Furthermore, the cost differential is not merely fiscal-it is ecological. Resistance is not an individual failure; it is a societal collapse.
Paige Basford
i just want to say that i used to hate taking antibiotics because they made me so nauseous… but then my doctor switched me to azithromycin and it was a game changer. one pill a day for five days? yes please. also, i started taking a probiotic with it and my stomach didn’t explode. i know it sounds dumb but it really helped. also, if you’re on doxycycline, don’t lie down for an hour after-you’ll regret it. trust me. i learned the hard way. 😅
Ankita Sinha
I’ve been studying this for my microbiology class and honestly, it’s wild how much we take for granted. Clavulanate doesn’t kill bacteria-it’s like a saboteur disabling their defense system. It’s not magic, it’s evolution. Bacteria learned to fight amoxicillin, so we built a countermeasure. But now they’re learning to fight clavulanate too. It’s an arms race. And we’re losing because we overuse. Every time someone takes an antibiotic for a cold, we’re feeding the monster. We need to treat antibiotics like diamonds, not candy.
Kenneth Meyer
There’s a quiet dignity in knowing when to stop. When the body is fighting, antibiotics are just a bridge. They don’t heal you. Your immune system does. The real question isn’t which drug to take-it’s whether you’re listening to your body. If you’re still sick after Augmentin, maybe it’s not about stronger medicine. Maybe it’s about rest. Maybe it’s about hydration. Maybe it’s about letting the body do what it was designed to do. We’ve forgotten that healing isn’t always a chemical solution. Sometimes, it’s just silence.
Danielle Mazur
The FDA’s warning regarding fluoroquinolones is not merely precautionary-it is a direct consequence of institutional negligence. The pharmaceutical industry’s prioritization of profit over patient safety has led to the normalization of high-risk therapeutics for low-risk conditions. The widespread use of ciprofloxacin for uncomplicated UTIs constitutes a public health failure. Regulatory oversight has been systematically undermined by lobbying and the erosion of evidence-based guidelines. This is not medicine. It is commodified risk.