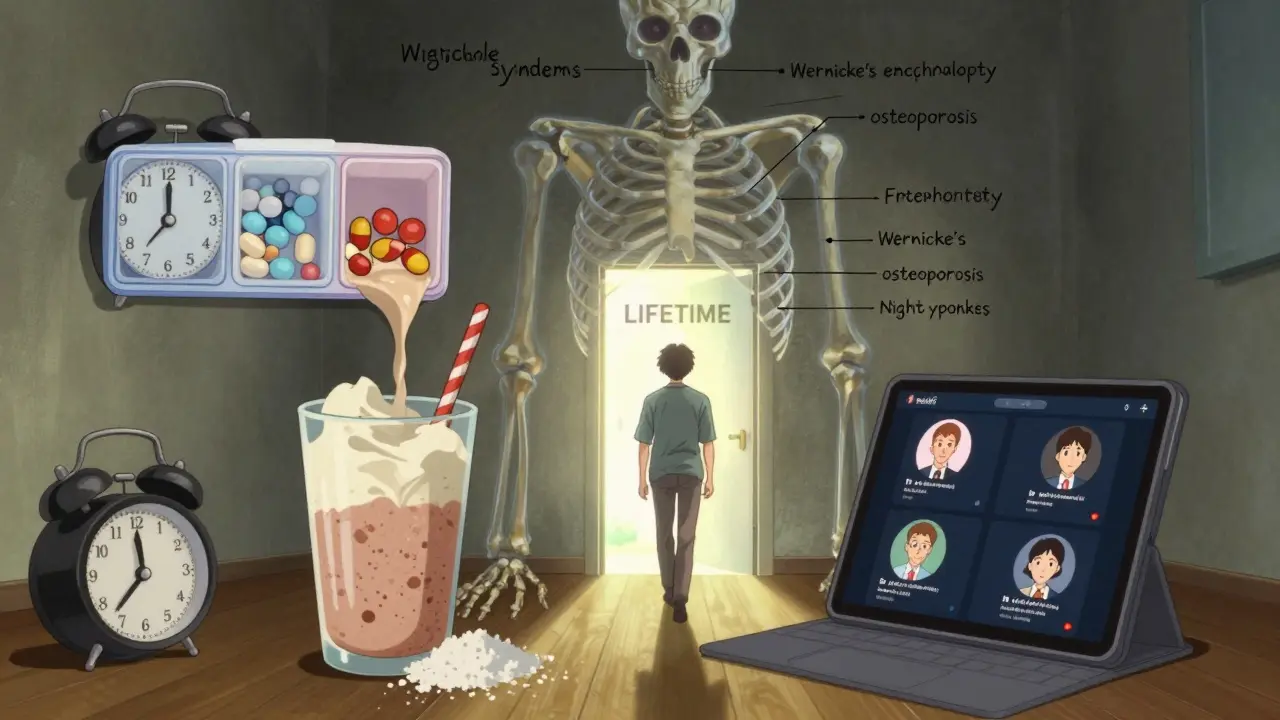
After weight loss surgery, your body doesn’t just lose fat-it loses its ability to absorb the nutrients it needs to survive. That’s not a side effect. It’s a biological reality. If you’ve had a gastric bypass, sleeve gastrectomy, or another bariatric procedure, your stomach is smaller, your intestines are rerouted, and your body can no longer pull in vitamins and minerals the way it used to. Without the right supplements, you’re not just at risk for fatigue or hair loss-you’re at risk for nerve damage, bone fractures, blindness, and even death.
Why Standard Multivitamins Won’t Cut It
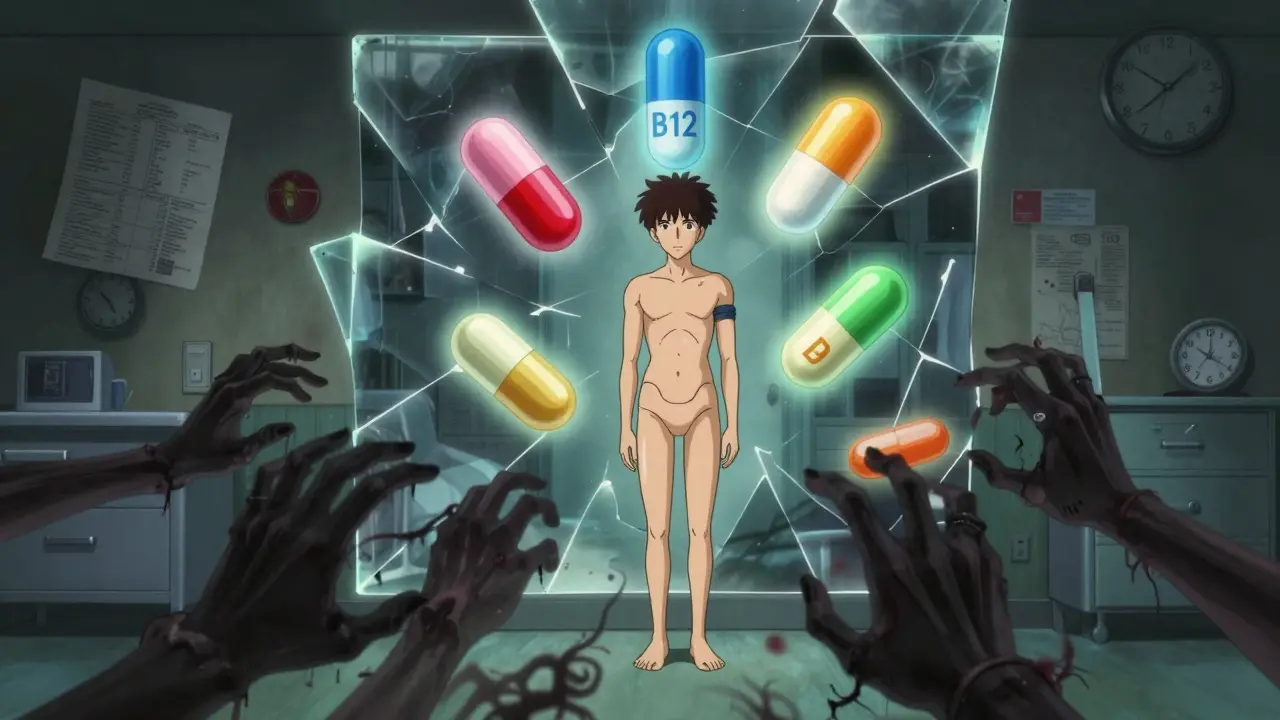
You might think, "I’ll just take my regular one-a-day multivitamin." That’s a dangerous assumption. Standard supplements are designed for people with fully functioning digestive systems. After bariatric surgery, your body can’t absorb them properly. Iron from a regular pill? Mostly wasted. Vitamin B12? Your stomach no longer makes the acid needed to release it from food. Calcium? Your body can’t absorb carbonate forms without stomach acid. The American Society for Metabolic and Bariatric Surgery (ASMBS) has been clear since 2006: bariatric patients need specialized, high-potency supplements. These aren’t fancy marketing gimmicks. They’re medical necessities. A 2019 review in OAE Publishing found that without proper supplementation, 60% of gastric bypass patients develop vitamin B12 deficiency within the first year. Nearly half develop folic acid deficiency. And vitamin D? One in eight will become deficient. These aren’t rare cases-they’re the norm if you skip the right vitamins.What You Actually Need to Take (By the Numbers)
Here’s what the science says you need daily, based on ASMBS 2019 guidelines and follow-up studies from Mayo Clinic and UVA Health:- Iron: At least 18 mg per day-preferably as ferrous fumarate, not sulfate, because it’s easier on your stomach.
- Vitamin B12: 500-1,000 mcg daily. Sublingual (under-the-tongue) or liquid forms work best. Some patients need injections, but most can manage with high-dose oral supplements.
- Calcium: 1,000-1,200 mg total per day, split into two or three doses of 500-600 mg each. Must be calcium citrate, never carbonate.
- Vitamin D3: 3,000 IU daily. Many patients start with levels below 20 ng/mL before surgery. That’s severely deficient. You’ll need this for life.
- Vitamin A: 5,000-10,000 IU daily. Fat-soluble, so absorption depends on bile flow-something that’s disrupted after bypass surgery.
- Thiamine (B1): 12 mg daily. Often overlooked, but critical. Deficiency can cause Wernicke’s encephalopathy-a neurological emergency.
- Folic Acid: 400-800 mcg daily. Especially important for women of childbearing age.
That’s not one pill. That’s often four to six. And you can’t just take them all at once. Calcium can’t be absorbed in doses over 600 mg. Vitamin D needs fat to be absorbed-so take it with food. Iron causes constipation and nausea-take it with vitamin C to help absorption and reduce side effects.
Different Surgeries, Different Needs
Not all bariatric surgeries are the same. Your supplement plan must match your procedure.- Roux-en-Y Gastric Bypass (RYGB): Highest risk for B12, iron, calcium, and fat-soluble vitamins (A, D, E, K). Malabsorption is built into the surgery. You need the strongest regimen.
- Sleeve Gastrectomy: Less malabsorption, but still significant. Iron and B12 deficiencies are common because the part of the stomach that produces acid and intrinsic factor (needed for B12 absorption) is removed. Vitamin D deficiency affects up to 50% of sleeve patients.
- Adjustable Gastric Band: Least malabsorptive, but still requires supplementation. Vitamin D deficiency is the most common issue here.
- Biliopancreatic Diversion with Duodenal Switch (BPD/DS): Most aggressive. Requires double or triple the doses of fat-soluble vitamins and protein supplements. Many patients need weekly B12 injections.
One size does not fit all. If your clinic gives you the same supplement list for every patient, ask for a better plan. Your surgery type determines your risk.

Form Matters-Chewables, Liquids, and Why Pills Don’t Work
For the first 3 to 6 months after surgery, your stomach is tiny. A regular pill might get stuck. Or worse-it might not dissolve at all. That means you’re swallowing money and risking deficiency.- Use chewable or liquid vitamins during recovery. Many patients report better tolerance and absorption.
- Look for bariatric-specific brands that offer softgels or powders you can mix into shakes.
- Some patients switch to liquid B12 after struggling with pills. One Reddit user, "BariatricWarrior2022," said his nerve pain disappeared within three months of switching to sublingual B12.
- Avoid large, hard tablets. Even if they say "easy to swallow," they’re not designed for post-op stomachs.
Some popular brands like Nature’s Bounty Bariatric Formula get high ratings for small pill size-but users consistently complain the calcium content is too low. You’ll likely need a separate calcium supplement. Kirkland Signature (Costco) and Bariatric Fusion offer higher-dose options, but always check the label.
Adherence Is the Real Problem
You might start strong. You buy the vitamins. You take them daily. You feel better. Then life happens. You miss a week. You forget. You think, "I’m fine." Here’s the hard truth: only 30-50% of patients stick with their vitamin regimen after five years. That’s according to a 2023 review in Clinical Obesity. And that’s why so many people end up back in the hospital-with anemia, osteoporosis, or neurological damage.- Use a pill organizer with morning, afternoon, and night slots.
- Set phone alarms. One alarm for calcium, one for iron, one for B12.
- Keep vitamins next to your toothbrush or coffee maker-places you already go daily.
- Join a support group. Reddit’s r/bariatrics has over 125,000 members. You’re not alone.
Iron supplements cause constipation. That’s common. Switch from ferrous sulfate to ferrous fumarate. Drink more water. Add magnesium. Don’t quit.
Testing Is Non-Negotiable
You can’t guess if you’re deficient. You need blood tests.- Get tested every 3-6 months for the first two years after surgery.
- After that, test annually-at minimum.
- Ask for: iron studies (ferritin, transferrin saturation), vitamin B12, folate, vitamin D, calcium, and thiamine.
- Don’t accept a "normal" result if you still feel tired, dizzy, or numb. Levels can be in the "low normal" range and still cause damage.
Dr. Kelly O’Donnell from UVA Health says vitamin deficiencies can cause "serious, irreversible" damage. Nerve damage from B12 deficiency? Can’t be undone. Bone loss from low vitamin D? Can’t be reversed without years of aggressive treatment. Prevention isn’t optional-it’s survival.
Cost and Access Are Real Barriers
A full bariatric supplement regimen can cost $30-$60 a month. For patients without insurance, that’s a burden. Some programs offer samples or discounts. Some pharmacies have generic bariatric lines. Ask your dietitian. Don’t skip vitamins because you can’t afford the brand name. Look for Costco’s Kirkland, or store brands that meet ASMBS specs.And if your surgeon doesn’t give you a written plan? Demand one. If your clinic doesn’t offer follow-up nutrition counseling? Find another provider. Your life depends on this.
What Happens If You Skip Them?
Let’s be blunt. Skipping bariatric vitamins doesn’t just mean you’ll feel sluggish. It means:- B12 deficiency: Numbness in hands and feet, memory loss, depression, balance problems. Can lead to permanent nerve damage.
- Vitamin D deficiency: Bone pain, muscle weakness, increased fracture risk. Osteoporosis can develop in just a few years.
- Iron deficiency: Fatigue, pale skin, shortness of breath, heart palpitations. Can lead to anemia requiring transfusions.
- Thiamine deficiency: Confusion, vision changes, vomiting, ataxia. Can cause Wernicke’s encephalopathy-a medical emergency that can kill.
- Vitamin A deficiency: Night blindness, dry eyes, increased infection risk.
These aren’t hypotheticals. They’re documented outcomes in medical journals. And they’re preventable.
What’s Next?
The future of bariatric nutrition is getting smarter. Some clinics are starting to use genetic testing to predict who’s at higher risk for certain deficiencies. Apps are being developed to remind you to take pills and schedule blood tests. Once-daily formulations are coming-but they’re not here yet.Right now, your job is simple: take your vitamins. Every day. No excuses. Your body changed. Your nutrition must change too. You didn’t have surgery to become sick-you had it to live better. That only happens if you protect your health with the right supplements.
Do I really need bariatric vitamins if I eat well?
Yes. Even the healthiest diet can’t replace what your body can no longer absorb. After gastric bypass or sleeve surgery, your digestive system is physically altered. You can eat perfect meals, but without supplements, your body can’t access the nutrients. Food alone is not enough.
Can I take regular multivitamins instead of bariatric ones?
No. Regular multivitamins contain far too little of the nutrients you need. For example, most contain only 12 mg of iron and 2.4 mcg of B12-far below the 18 mg and 500-1,000 mcg you require. They also use calcium carbonate, which your body can’t absorb without stomach acid. Bariatric vitamins are specifically designed to meet your post-surgery needs.
Why do I need to split my calcium doses?
Your body can only absorb about 500-600 mg of calcium at a time. If you take 1,200 mg all at once, half of it passes through unused. Splitting it into two or three doses-preferably with meals-ensures maximum absorption. Calcium citrate is best because it doesn’t need stomach acid to be absorbed.
What if I can’t swallow pills after surgery?
Use chewable, liquid, or powder forms. Many bariatric vitamin brands offer these options. Some patients mix powdered vitamins into protein shakes or yogurt. Your dietitian can help you find a form that works. Don’t give up-there’s always an alternative.
How long do I need to take these vitamins?
For life. Bariatric surgery permanently changes how your body absorbs nutrients. Stopping supplements-even after years of feeling fine-can lead to dangerous deficiencies. Studies show that patients who stop taking vitamins after five years are at high risk for bone disease, neurological damage, and anemia.
Can I get too much of a vitamin?
Yes, especially with fat-soluble vitamins like A, D, E, and K. Vitamin A toxicity can occur with chronic high doses above 10,000 IU daily without medical supervision. Always follow your provider’s dosage. Blood tests help ensure you’re not overdosing. Water-soluble vitamins like B12 and C are safer because excess is excreted.
Why do I need to test my vitamin levels so often?
Deficiencies develop slowly and silently. You might not feel symptoms until damage is already done. Blood tests catch problems early. For example, ferritin (iron storage) can drop for months before you feel tired. Regular testing lets your team adjust your doses before you get sick.
Sarthak Jain
bro i thought i was doing good till i read this. i’ve been taking my bariatric vitamins but i mix em in protein shakes and sometimes forget the calcium. now i’m paranoid i’m gonna end up with nerve damage 😅
Sinéad Griffin
AMERICA IS THE ONLY COUNTRY THAT DOES THIS RIGHT 🇺🇸💥 if you’re not taking 3000 IU of D3 and 1000mcg B12 sublingual, you’re just playing russian roulette with your nerves. #BariatricPride
Edward Stevens
so let me get this straight… we’re telling people to take 6 different pills a day, at specific times, with food, and not all together… and you’re surprised only 30% stick with it? 🤦♂️
Wade Mercer
you people are so careless. you get surgery to fix your life, then you treat your body like a broken vending machine. if you can’t commit to 6 pills a day, maybe you shouldn’t have had the surgery in the first place.
Natalie Koeber
did you know the FDA allows vitamin companies to lie about dosage because they’re classified as ‘supplements’? they’re all just sugar pills with glitter. the real reason you’re deficient is because the pharmaceutical industry wants you dependent on expensive ‘bariatric’ brands. #VitaminConspiracy
Rulich Pretorius
the body doesn’t care about your intentions. it only responds to what you give it. after surgery, your digestive system is not a suggestion-it’s a rewrite. you don’t get to negotiate with biology. take the vitamins. track your labs. show up for yourself. this isn’t about discipline-it’s about respect.
Tim Bartik
my wife took her calcium with coffee and thought she was fine. 18 months later, she broke her wrist sneezing. now she takes it with lunch, chews it, and yells at me when i forget to remind her. don’t be her. don’t be me.
jeremy carroll
you got this. i was at my worst after surgery-constipated, tired, forgot my pills for 3 weeks. switched to chewables, set 3 alarms, and now i’m 3 years in and feeling better than i did in my 20s. it’s a grind, but it’s worth it. you’re not alone 💪
Daniel Thompson
as a former bariatric patient and current clinical nutritionist, I must emphasize that calcium citrate is non-negotiable. The use of carbonate is a documented error in over 60% of non-specialized regimens. Please consult your dietitian before self-prescribing.
Alexis Wright
you call this advice? this is just fear-mongering dressed up as science. 60% deficiency? 50% non-compliance? that’s not a medical crisis-that’s a systemic failure of the bariatric industry to provide sustainable care. they sell you surgery, then sell you $60/month pills and call it ‘lifelong care.’ it’s a pyramid scheme with a stethoscope.
Daniel Wevik
if you’re reading this and you’re struggling with adherence-stop. breathe. you’re not failing. your system is just asking for a better setup. try a pill organizer with alarms. switch to liquid B12. find your tribe on r/bariatrics. this isn’t about perfection-it’s about persistence. you’re already ahead of 90% of people who never even tried.
Rich Robertson
in South Africa, we don’t have access to branded bariatric vitamins. we use generic calcium citrate, B12 injections from the public clinic, and D3 from the pharmacy next to the taxi rank. you don’t need fancy labels-you need consistency. if you can get your hands on a pill, take it. if you can’t, talk to your clinic. your life isn’t dependent on the brand-it’s dependent on you.