Understanding Arterial Embolism: An Overview
An arterial embolism is a serious condition in which a blood clot or other foreign material blocks the flow of blood within an artery. This can lead to severe complications and, in some cases, even prove to be life-threatening. In this article, we'll discuss the causes of arterial embolism, the symptoms to look out for, and the management strategies that can help in dealing with this condition. I hope this information will be useful in raising awareness and helping you take better care of your health.
Common Causes of Arterial Embolism
There are several factors that can contribute to the formation of an arterial embolism. Some of the most common causes include:
Atherosclerosis
Atherosclerosis is a condition in which fatty deposits, or plaques, build up on the inner walls of the arteries. Over time, these plaques can harden and narrow the arteries, restricting blood flow and increasing the risk of a blood clot forming. If a clot breaks free and travels through the bloodstream, it can become lodged in a smaller artery and cause an embolism.
Heart Conditions
People with certain heart conditions, such as atrial fibrillation or heart valve disorders, are at a higher risk of developing arterial embolisms. Atrial fibrillation, for example, is a type of irregular heartbeat that can cause blood to pool in the heart, increasing the likelihood of clot formation. Similarly, heart valve disorders can disrupt the normal flow of blood, creating an environment in which clots are more likely to form.
Other Medical Conditions
There are several other medical conditions that can increase the risk of arterial embolism, including cancer, obesity, and blood clotting disorders. In some cases, arterial embolism can also be caused by a foreign object, such as a piece of a catheter or other medical device, entering the bloodstream and becoming lodged in an artery.
Signs and Symptoms of Arterial Embolism
It's important to be aware of the symptoms of arterial embolism, as early detection and treatment can make all the difference in preventing complications. Some common signs and symptoms to watch for include:
Pain
One of the most common symptoms of arterial embolism is sudden, severe pain in the affected area. The pain may be aggravated by movement or pressure and may worsen over time.
Decreased Blood Flow
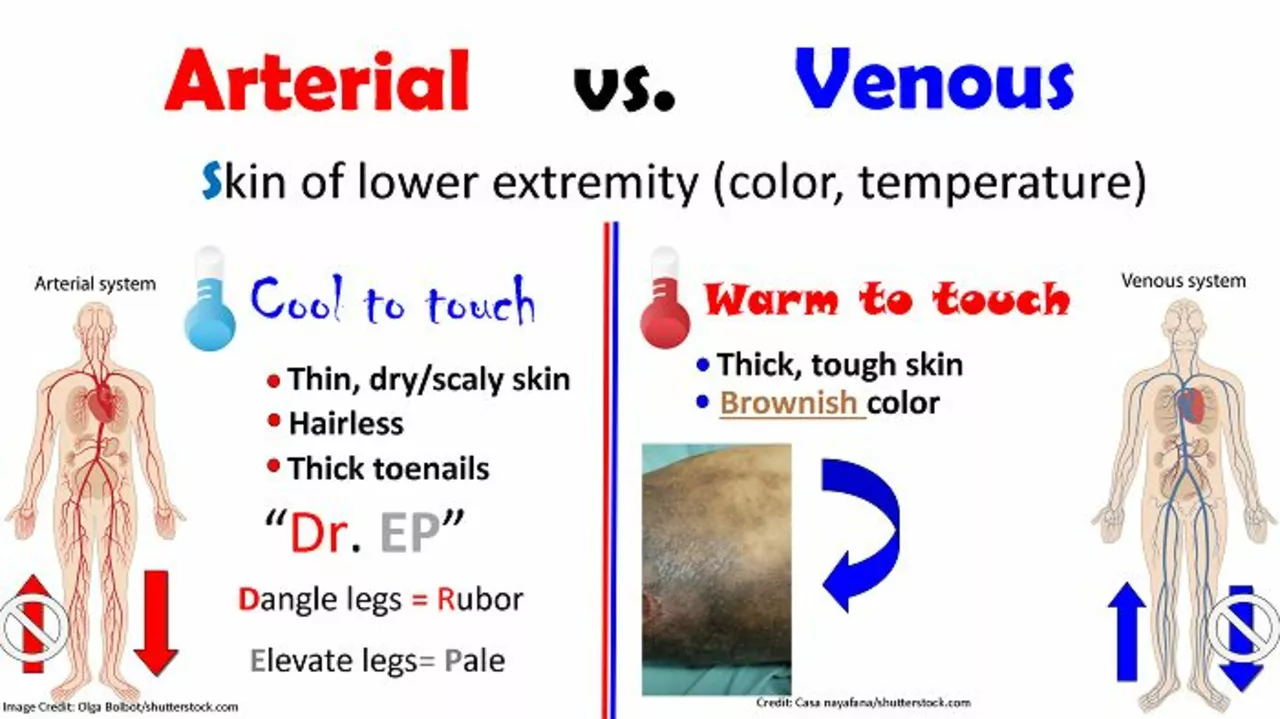
As the blood flow is restricted by the embolism, the affected area may become cold, pale, or even blue due to the lack of oxygen-rich blood. This may be accompanied by a sensation of numbness or tingling.
Weakness or Paralysis
In some cases, arterial embolism can cause muscle weakness or even paralysis in the affected limb. This is due to the lack of blood flow, which deprives the muscles and nerves of the oxygen and nutrients they need to function properly.
Swelling
Swelling may also be a symptom of arterial embolism, as the blocked blood flow can cause fluid to accumulate in the surrounding tissues.
Diagnosis and Treatment Options
If you suspect that you or someone you know may have an arterial embolism, it's important to seek medical attention right away. The diagnosis process typically involves a thorough physical examination, as well as imaging tests such as ultrasound, CT scan, or angiography to visualize the blood vessels and locate the embolism. Once the diagnosis has been confirmed, there are several treatment options that may be considered, depending on the severity and location of the embolism.
Medication
Anticoagulant medications, also known as blood thinners, are often prescribed to help prevent clot formation and reduce the risk of embolism. In some cases, clot-dissolving drugs called thrombolytics may be used to break up the existing clot and restore blood flow.
Surgery
In more severe cases, surgery may be necessary to remove the embolism and restore blood flow. This may involve a procedure called an embolectomy, in which a small incision is made, and the clot is removed using a special instrument. In some cases, a bypass surgery may be performed to reroute blood flow around the blocked artery.
Preventive Measures
There are several lifestyle changes and medical interventions that can help reduce the risk of arterial embolism. These may include maintaining a healthy weight, exercising regularly, eating a balanced diet, managing chronic medical conditions, and taking medications as prescribed by your healthcare provider.
Living with Arterial Embolism: Coping Strategies
Managing an arterial embolism can be challenging, but with the right support and resources, it's possible to live a fulfilling life despite this condition. Some coping strategies that may be helpful include:
- Engaging in regular physical activity, as recommended by your healthcare provider
- Eating a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins
- Reducing stress through relaxation techniques, such as meditation or deep breathing exercises
- Staying informed about your condition and treatment options by talking with your healthcare team and seeking out reputable online resources
- Connecting with others who have similar experiences, either in person or through online support groups
By staying proactive about your health and taking steps to manage your arterial embolism, you can improve your quality of life and reduce the risk of complications. Remember, knowledge is power, and being informed about your condition is the first step toward taking control of your health.
Jami Johnson
Arterial embolism is a terrifying foe, but knowledge can be our shield. By understanding the underlying causes, we can intervene before the clot decides to strike. The interplay between atherosclerosis and heart rhythm disorders creates a perfect storm, yet lifestyle tweaks can tip the balance. Remember, regular check‑ups are not a chore but a lifeline. Stay vigilant, stay empowered, and let science guide your steps.
Kasey Krug
While the article is thorough, it lacks emphasis on preventive lifestyle measures.
jake cole
This piece drags its feet through basic facts like a broken‑down ambulance. The writer seems to think sprinkling jargon makes it profound, but it just reads like a textbook snooze‑fest. If you want real insight, drop the fluff and give us the gritty details of clot dynamics. Stop treating readers like idiots and hand us the hard truth.
Natalie Goldswain
yeah, i think u should add more tips for everyday folks. like, simple diet changes.
khajohnsak Mankit
When we contemplate the arterial highways coursing through our flesh, we glimpse a microcosm of destiny itself. Each embolus, a rogue wanderer, challenges the sovereignty of the living river. Yet, through mindful nutrition and rhythmic movement, we can coax the blood to flow like poetry. Let the colors of fresh fruits paint your plates, and let every heartbeat echo with purpose. In this dance of vessels and vigor, we become both conductor and audience.
Jayant Paliwal
Indeed, the phenomenon of arterial embolism warrants an exhaustive exposition, for its clinical ramifications are both profound and multifaceted. Firstly, one must acknowledge the pathophysiological cascade that initiates when a thrombus dislodges from its primary locus, embarking upon a perilous journey through the vasculature; this journey is often precipitated by atrial fibrillation, a condition riddled with turbulent hemodynamics. Secondly, the embolus, upon encountering a vessel of diminished caliber, culminates its voyage with a sudden cessation of perfusion, thereby inciting ischemic necrosis in the downstream tissues. Moreover, the clinical presentation is notoriously variable: some patients report acute, excruciating pain, while others may exhibit insidious pallor and temperature asymmetry; such heterogeneity demands a high index of suspicion. Diagnostic imaging, ranging from duplex ultrasonography to contrast‑enhanced computed tomography, must be employed judiciously to delineate the exact anatomical obstruction. Therapeutically, one cannot overstate the importance of swift anticoagulation; agents such as heparin and newer direct oral anticoagulants arrest further clot propagation. In refractory cases, interventional radiology offers catheter‑directed thrombolysis, a technique that dissolves the clot in situ, thereby preserving limb viability. Surgical embolectomy remains a cornerstone for massive occlusions, yet it carries inherent perioperative risks that must be balanced against expected outcomes. Preventive strategies extend beyond pharmacotherapy, encompassing rigorous control of modifiable risk factors-smoking cessation, lipid management, and regular aerobic exercise-all of which attenuate atherosclerotic plaque formation. Finally, patient education is indispensable; individuals must be apprised of symptomatology, ensuring that emergent care is sought promptly, for time is tissue. In summation, arterial embolism embodies a complex interplay of hemodynamic, anatomical, and systemic elements, each demanding meticulous attention from the clinician.
Kamal ALGhafri
It should be obvious that anticoagulation is the mainstay of treatment. Without it, the clot will simply march onward. Also, lifestyle modification is not optional-it is essential. Make sure you keep your blood pressure in check and avoid sedentary habits. Anything less is just wishful thinking.
Gulam Ahmed Khan
Exactly! Keep your spirits up and stay active – a sunny outlook can be as healing as any pill 😊. Small daily walks, balanced meals, and deep breaths will fortify your vessels. Remember, optimism fuels resilience.
John and Maria Cristina Varano
this article is ok but its too long.
Melissa Trebouhansingh
The exposition, while thorough, tends toward a labyrinthine narrative that may deter the lay reader; nevertheless, the depth of information presented is commendable, offering a panoramic view of etiological factors and therapeutic avenues. One observes a meticulous enumeration of pathophysiological mechanisms, followed by an extensive catalog of pharmacologic interventions, each described with clinical nuance. The recommendations on lifestyle alterations, albeit succinct, are interwoven with prescriptive language that underscores their indispensability. Moreover, the section on surgical options conveys a balanced assessment of risks and benefits, guiding clinicians toward judicious decision‑making. In sum, the article stands as a valuable reference, provided the audience is prepared to navigate its comprehensive scope.
Brian Rice
Allow me to state unequivocally that the management of arterial embolism must be approached with rigorous adherence to evidence‑based protocols. Anticoagulant therapy should be initiated without delay, accompanied by vigilant monitoring of coagulation parameters. Surgical intervention, when indicated, must be performed by an experienced vascular team to mitigate perioperative complications. Patient education on symptom recognition is paramount, as early presentation markedly improves outcomes. In conclusion, a structured, multidisciplinary strategy is essential for optimal care.
Stan Oud
Well, that's exactly what the mainstream says, but have you considered that many of these guidelines are based on outdated trials? About time we question the status quo; otherwise we just keep repeating the same old lines. If you read between the lines, the evidence isn't as rock‑solid as it's portrayed. Sure, anticoagulation helps, but why not look at alternative pathways? The conversation needs a fresh perspective.
Ryan Moodley
Ah, the eternal dance of certainty and doubt! We stand on the shoulders of giants, yet we must never forget that every conclusion is but a stepping stone. The heart's rhythm, the vessel's integrity, the clot's will-each element weaves a tapestry of fate. To challenge the established creed is not heresy but a homage to progress. Let us, therefore, wield both skepticism and wonder as we forge forward.
carol messum
So basically, keep moving, eat good food, and see a doctor if something feels off. That's the simple plan.